- New stuff to read and discuss
- What patients say
- Clinic / online appointments
- Why the diagnosis of a psychosomatic illness is often a misdiagnosis
- Vascular Compression Syndromes
- Do you have questions?
- Checklist vascular compression syndromes
- Description of your symptoms
- Researchers from the Mayo Clinic confirm my concept of the Midline Congestion Syndrome
- Explanation of gender-specific differences in the clinical symptoms of abdominal vascular compression syndromes: varicocele and penile/testicular pain – their main manifestation in men.
- Varicocoele is predominantly caused by left renal vein compression
- Musculoskeletal pecularities of female puberty
- Lordosis /Swayback- Origin of many abdominal compression syndromes
- Bending of a straight vein compels its narrowing
- The lordogenetic midline congestion syndrome
- Neurological consequences of the midline congestion syndrome
- Successful treatment of a teenage girl who was unable to eat due to extreme postprandial pain and unable to walk due to spasticity in her left leg
- Severe ataxia in a young woman with severe spinal congestion – complete resolution after decompression of the left renal vein
- All compression syndromes are one: the spectrum of lordogenetic compressions
- Nutcracker-Syndrome is a misnomer! Lordogenetic left renal vein compression is a more appropriate name!
- May-Thurner-constellation (May-Thurner-syndrome, Cockett’s syndrome)
- Midline (congestion) syndrome
- Pelvic congestion syndrome
- Celiac Trunk Compression / Dunbar syndrome / MALS / Arcuate ligament syndrome
- Wilkie-Syndrome / Superior-mesenteric-artery-syndrome
- Compression of the vena cava inferior
- Evlauation of vascular compressions with the PixelFlux-method
- Connective tissue disorders predispose to multiple compressions
- Postural tachycardia syndrome (POTS) – the hemodynamic consequence of vascular compression syndromes and loose connective tissue
- Restless legs-a little known symptom of abdominal vascular compression syndromes
- Pudendal neuralgia in vascular compression syndromes
- A new sonographic sign of severe orthostatic venous pooling
- Migraine and Multiple Sclerosis
- Hemodynamic effect on cerebral perfusion in patients with multiple localised vascular compression.
- Treatment of vascular compression syndromes
- Fatal errors in the treatment of vascular compression syndromes
- Risks of stents in venous compression syndromes
- Surgical treatment of abdominal compression syndromes: The significance of hypermobility‐related disorders
- Nutcracker and May-Thurner syndrome: Decompression by extra venous tube grafting and significance of hypermobility related disorders
- Our surgical treatment of vascular compressions
- Chronic regional pain syndrome (CRPS) caused by venous compression and mechanical irritation of the coeliac plexus
- Vascular compression syndromes I recently detected
- Kaleidoscope of instructive cases
- Ultrasound Diagnostics
- Profile
- Functional colour Doppler ultrasound – how I do it
- Perfusion Measurement – PixelFlux-method
- Research
- Publications
- Nutcracker and May-Thurner syndrome: Decompression by extra venous tube grafting and significance of hypermobility related disorders
- Papers authored by Th. Scholbach
- Publications
- Inauguration of measurements of the tissue pulsatility index in renal transplants
- From nutcracker phenomenon to midline congestion syndrome and its treatment with aspirin
- First sonographic tissue perfusion measurement in renal transplants
- First sonographic bowel wall perfusion measurement in Crohn disease
- First sonographic renal tissue perfuison measurement
- First sonographic measurement of renal perfusion loss in diabetes mellitus
- PixelFlux measurements of renal tissue perfusion
- Why I prefer not to publish in journals but in the Internet
- Vessel stretching in nephroptosis – an important driver of complaints
- Publications
- Expertise
- Bornavirus Infection
- Scientific cooperation
- Cookie Policy
- Data protection
- Cookie Policy (EU)
- Impressum

A new sonographic sign of severe orthostatic venous pooling
A new sonographic sign of severe orthostatic venous pooling
Many patients with vascular compression syndromes suffer from pain in the lower abdomen radiating towards the legs sometimes with a swelling of the legs or the outer genitals. In women dyspareunia is a common debilitating consequence of massive congestion of the inner and outer genitals.
Some of these patients cannot tolerate to stand or sit for even a short time. To prevent fainting, they must sit or lay down in order to recover from rapidly increasing tachycardia, brain fog, dizziness, increasing pain in the lower abdomen and in the legs and to prevent fainting.
In these patients it is important to define the degree of orthostatic perfusion drop which means to determine the volume flow differences in the upper abdominal aorta when these patients transit from a horizontal to an erect posture of the trunk. Very often is not only difficult for them to stand but also to sit. From a physical perspective standing and sitting bear important similarities-gravitational traction is in parallel with the orientation of the trunk. Thus, gravitation pulls the blood down towards the pelvis and-while standing-into the legs and feet.
I report here on a new sign of severe venous pooling in the pelvis in a patient which could not tolerate to stand for a short while. Even while walking around during her work as a hairdresser, she could not work longer than 2 hours and then needed a rest because of the above-mentioned symptoms.
The volume drop within the aorta was extreme as soon as the patient turned from a horizontal to a vertical posture.
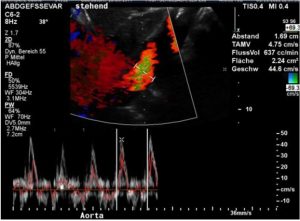
The aortic perfusion volume dropped from 2677 mL/min to only 637 mL/min which is a orthostatic reduction of the circulating blood flow volume by 76%!
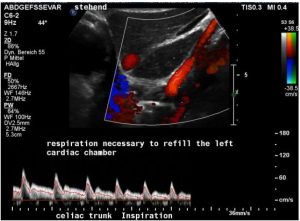
In this patient I observed an impressive heartbeat by heartbeat reduction of the cardiac output evaluated by the Doppler signal within the coeliac trunk in a standing posture.
In inspiration a steady and continuous linear decline of the cardiac output was observed. Given the constant trans-sectional diameter of the coeliac trunk the reduction of the flow velocity corresponds directly to the reduction of the cardiac output from 100% to 56% in the short time span of only 6 heartbeats:
| Heartbeat | Flow velocity (cm/s) | Relative reduction of flow volume |
| 1. beat | 91,7 | 100% |
| 2. beat | 77,5 | 84% |
| 3. beat | 65,8 | 72% |
| 4. beat | 60,8 | 66% |
| 5. beat | 52,5 | 57% |
| 6. beat | 51,7 | 56% |
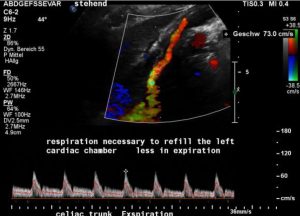
This effect was only visible inspiration but not in expiration.
My explanation for this different reaction of the circulation onto the position of the diaphragm:
In deep inspiration the diaphragm is contracted at maximum to enlarge the thoracic volume but simultaneously exerts maximum pressure onto the abdominal cavity. Then the diaphragm is squeezing the bowel into the pelvis. Not only the abdominal organs are pushed down but the high pressure in the abdomen which is produced by the down pressing of the diaphragm puts counterpressure onto the venous return from the pelvis. Thus, as soon as the patient inhales deeply and holds the diaphragm in this position suddenly only little blood can return from the pelvis to refill the heart. Thus, the filling of the left cardiac chamber is significantly reduced only by holding the diaphragm in a deep inspiratory position. So, heartbeat by heartbeat the cardiac output declines at a staggering rate what is shown in the ultrasound image and the table above.
In expiration the diaphragm is maximally relaxed allowing it to resume its dome shaped position. This reduces the lung volume but increases the abdominal volume thus decreases the pressure onto the blood vessels which in turn allows an easier upstream of blood from the pelvis towards the heart. This, from my perspective, is the reason that in the same patient in expiration no dropping cardiac output can be observed.
This may be a valuable and simple sign to estimate the severity of venous pooling and the distensibility of pelvic veins in patients with connective-tissue disorders and a severe orthostatic intolerance resulting in postural tachycardia syndrome, fainting , brain fog , inability to stand or sit for even a short while, increasing abdominal pain and tension in the legs.
Even without ultrasound this could be eventually used as a clinical test to evaluate a patient with orthostatic tachycardia. The patient may simply be asked to stand upright and then should be observed while deeply inhaling and holding the diaphragm in comparison to holding the diaphragm in in expiration position. It can be observed expected that the circulatory response with the need to sit down or lay down is more urgent during the inspiratory arrest of the diaphragm compared to the expiration arrest.