- New stuff to read and discuss
- What patients say
- Clinic / online appointments
- Why the diagnosis of a psychosomatic illness is often a misdiagnosis
- Vascular Compression Syndromes
- Do you have questions?
- Checklist vascular compression syndromes
- Description of your symptoms
- Researchers from the Mayo Clinic confirm my concept of the Midline Congestion Syndrome
- Explanation of gender-specific differences in the clinical symptoms of abdominal vascular compression syndromes: varicocele and penile/testicular pain – their main manifestation in men.
- Varicocoele is predominantly caused by left renal vein compression
- Musculoskeletal pecularities of female puberty
- Lordosis /Swayback- Origin of many abdominal compression syndromes
- Bending of a straight vein compels its narrowing
- The lordogenetic midline congestion syndrome
- Neurological consequences of the midline congestion syndrome
- Successful treatment of a teenage girl who was unable to eat due to extreme postprandial pain and unable to walk due to spasticity in her left leg
- Severe ataxia in a young woman with severe spinal congestion – complete resolution after decompression of the left renal vein
- All compression syndromes are one: the spectrum of lordogenetic compressions
- Nutcracker-Syndrome is a misnomer! Lordogenetic left renal vein compression is a more appropriate name!
- May-Thurner-constellation (May-Thurner-syndrome, Cockett’s syndrome)
- Midline (congestion) syndrome
- Pelvic congestion syndrome
- Celiac Trunk Compression / Dunbar syndrome / MALS / Arcuate ligament syndrome
- Wilkie-Syndrome / Superior-mesenteric-artery-syndrome
- Compression of the vena cava inferior
- Evlauation of vascular compressions with the PixelFlux-method
- Connective tissue disorders predispose to multiple compressions
- Postural tachycardia syndrome (POTS) – the hemodynamic consequence of vascular compression syndromes and loose connective tissue
- Restless legs-a little known symptom of abdominal vascular compression syndromes
- Pudendal neuralgia in vascular compression syndromes
- A new sonographic sign of severe orthostatic venous pooling
- Migraine and Multiple Sclerosis
- Hemodynamic effect on cerebral perfusion in patients with multiple localised vascular compression.
- Treatment of vascular compression syndromes
- Fatal errors in the treatment of vascular compression syndromes
- Risks of stents in venous compression syndromes
- Surgical treatment of abdominal compression syndromes: The significance of hypermobility‐related disorders
- Nutcracker and May-Thurner syndrome: Decompression by extra venous tube grafting and significance of hypermobility related disorders
- Our surgical treatment of vascular compressions
- Chronic regional pain syndrome (CRPS) caused by venous compression and mechanical irritation of the coeliac plexus
- Vascular compression syndromes I recently detected
- Kaleidoscope of instructive cases
- Ultrasound Diagnostics
- Profile
- Functional colour Doppler ultrasound – how I do it
- Perfusion Measurement – PixelFlux-method
- Research
- Publications
- Nutcracker and May-Thurner syndrome: Decompression by extra venous tube grafting and significance of hypermobility related disorders
- Papers authored by Th. Scholbach
- Publications
- Inauguration of measurements of the tissue pulsatility index in renal transplants
- From nutcracker phenomenon to midline congestion syndrome and its treatment with aspirin
- First sonographic tissue perfusion measurement in renal transplants
- First sonographic bowel wall perfusion measurement in Crohn disease
- First sonographic renal tissue perfuison measurement
- First sonographic measurement of renal perfusion loss in diabetes mellitus
- PixelFlux measurements of renal tissue perfusion
- Why I prefer not to publish in journals but in the Internet
- Vessel stretching in nephroptosis – an important driver of complaints
- Publications
- Expertise
- Bornavirus Infection
- Scientific cooperation
- Cookie Policy
- Data protection
- Cookie Policy (EU)
- Impressum

Severe abdominal pain and inability to perform even transcutaneous tube feeding due to a combination of intestinal malrotation and compression of the portal vein
I present a 24-year-old female patient who has lost 30kg in weight over the last 3 years because she was unable to eat enough due to extreme pain in her upper abdomen after eating. Even putting a double tube into her stomach and jejunum through the skin didn’t help. The patient could only tolerate 15ml/min of tube feeding for a maximum of 10 hours a day, so she continued to lose weight because she was only receiving 225 kcal per day.
The patient had surgery eight years ago for Wilkie syndrome, and doctors later discovered she had Nutcracker and May-Thurner syndromes. She had surgery for glioblastoma in 2022 and is now in remission and tumor free. A remnant from the brain operation include hearing loss on the right side and memory problems. Recently she has developed weakness in the left leg, and later also in the right leg, both of which are painful. After swallowing even a little bit of food or drink, she starts vomiting after two minutes.
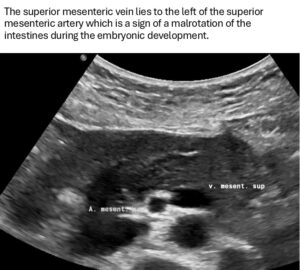
Her symptoms could be explained by the disturbed venous drainage from the small bowel since she had a malformation of her GI tract with a so-called malrotation of the foregut. This implies that the superior mesenteric vein is located left instead of right to the superior mesenteric artery. Thus, the mouth of the superior mesenteric vein into the splenic vein lies far more left compared to patients without this malformation.
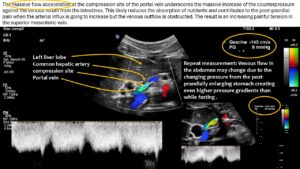
Since the common hepatic artery compressed the portal vein significantly with a flow acceleration to 147 cm/s the pressure within the splenic vein was completely transferred onto the venous return from the small bowel via the superior mesentric vein.
Moreover, the uptake of small amounts of food and even the balloon which blocks the transcutaneous catheter and prevents its dislocation were exerting pressure not only onto the superior mesenteric vein but also onto the left renal vein.
The left renal vein was severely compressed which is often referred to-albeit somewhat misleading-as nutcracker syndrome. The coexisting May-Thurner syndrome further exaggerated the pressurisation of veins in the left pelvic and abdominal hemisphere since the route via the left ovarian vein which usually helps to decrease the pressure inside the compressed left renal vein could not work properly due to the severe counterpressure from the pelvic mouth of the ovarian vein.
| Main Symptoms | Description |
| First main symptom | Vomiting, stomach ache |
| Second main symptom | Heavy legs |
| Third main symptom | Cramps in the hands, sweating |
| BMI | 16,00 |
The abdominal pain was most severe on the left side of the abdomen throughout the day at the level of 10/10. Other areas of the abdomen were also painful at the level of 7-8/10 during all day. The clinical examination revealed a cachectic patient with a transcutaneous 2-legged-feeding tube in the midline of the upper abdomen. Moreover, the entire abdomen was painful on palpation, and the patient was vomiting after an attempt to swallow 2 sips of water. Clinical examination showed definite signs of a Hypermobility Spectrum Disorder with a Beighton score of 9/9.
Sonographic findings:
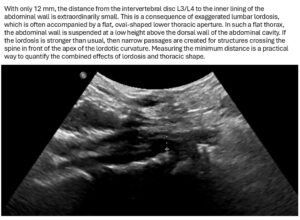
- Exaggerated lumbar lordosis
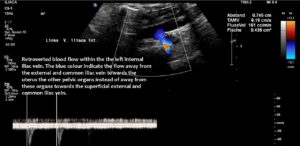
- Subtotal compression of the left common iliac vein with clinical consequences as frequent voiding, severe menstrual pain and pain and heaviness of the left leg- May-Thurner syndrome
- Low-grade compression of the vena cava at its root in front of the intervertebral disc L3/L4
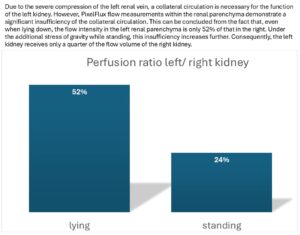
- Total compression of the left renal vein by the uplifted aorta in front of the aorta-maximum form of a so-called nutcracker syndrome
- Not yet diagnostic compression of the coeliac trunk-no median arcuate ligament syndrome
- Malrotation of the mesenteric vessels
- Severe compression of the portal vein by the common hepatic artery reducing the venous outflow from the small intestines and thus contributes to the maldigestion and malabsorption of the patient
- Extreme orthostatic right-sided nephroptosis
- Compensated additional orthostatic venous pooling by increasing heart rate-POTS with inability to stand for more than 5 minutes
- Reduced venous and arteial superior mesenteric flow volume
Correlation of the sonographic finding and the clinical symptoms
The persistent left-sided flank pain can be attributed to the severe compression of the left renal vein, resulting in elevated pressure within the entire vein, radiating towards the kidney and subsequently down the left ovarian vein towards the pelvis. Distended veins become painful.
The attempt to redirect the pressurised blood from the left renal vein via the left ovarian vein towards the pelvis proved unsuccessful due to the obstructed outflow from the left pelvic hemisphere, a consequence of the compression of the left common iliac vein (May-Thurner syndrome).
The accumulation of blood in the veins, particularly under the effect of gravitation during standing, forces the blood towards the lower hemisphere. This leads to the development of postural tachycardia syndrome, characterised by the inability to stand for more than a few minutes due to the need to rapidly recirculate the reduced available blood volume to maintain adequate perfusion of the brain, which otherwise would result in syncope due to critical cerebral hypoperfusion.
The patient’s inability to be fed via a transcutaneous feeding tube was due to a combination of two factors. Firstly, an inborn anomaly in the development of the gastrointestinal tract, and secondly, an acquired compression of the portal vein.
The patient was born with a malrotation of the foregut. This means that the positioning of the small bowel is not evenly distributed towards the left and right sides of the abdomen. Instead, the small intestines are located mainly on one side of the abdomen. In addition, the positions of the blood vessels of the mesentery were exchanged. Normally, the superior mesenteric vein enters the splenic vein on the right side of the superior mesenteric artery. In this patient, it enters left to the superior mesenteric artery.
The superior mesenteric vein and the splenic vein converge to form the portal vein. This vessel is typically of a relatively short length, given that the confluence of the superior mesenteric and splenic veins occurs in close proximity to the liver in most individuals. However, in this particular case, the portal vein exhibited a notable elongation, a consequence of the left-sided unification of the superior mesenteric and splenic veins. This anatomical variation potentially renders the portal vein more vulnerable to dislocation, making subsequent compression by the common hepatic artery easier. It should be noted that similar cases have been previously documented on this website, albeit in the absence of malrotation. In these cases, the compression was precisely at the point of unification between the two veins, namely the superior mesenteric and splenic veins. This may have resulted in a residual bypass from the superior mesenteric vein to the portal vein, thereby leading to a subtotal compression of the superior mesenteric vein.
All In this instance, the circumstances were somewhat divergent. The portal vein was of a greater length due to the unification of the splenic and superior mesenteric veins being in close proximity to the spleen. Consequently, there was a complete transfer of pressure from the compression site at the portal vein to both of these veins.
I have previously outlined the impact on the venous return from the small bowel with a 4D-PixelFlux volume flow measurement of the superior mesenteric vein and artery.
This showed that blood flow to the small bowel was reduced, probably because of the blockage. Moreover, this situation implies increased pressure in the superior mesenteric vein which was much wider than the accompanying superior mesenteric artery as a sign of the painful distension. An increase in intra-abdominal pressure, whether it occurs orally or via a feeding tube, can result in the onset of acute pain due to the subsequent rise in pressure within the mesenteric and renal veins on the left side of the body. This phenomenon is further compounded by the obstruction of venous outflow from the spleen, which can exacerbate discomfort in the region below the left rib cage.