- New stuff to read and discuss
- What patients say
- Clinic / online appointments
- Why the diagnosis of a psychosomatic illness is often a misdiagnosis
- Vascular Compression Syndromes
- Do you have questions?
- Checklist vascular compression syndromes
- Description of your symptoms
- Researchers from the Mayo Clinic confirm my concept of the Midline Congestion Syndrome
- Explanation of gender-specific differences in the clinical symptoms of abdominal vascular compression syndromes: varicocele and penile/testicular pain – their main manifestation in men.
- Varicocoele is predominantly caused by left renal vein compression
- Musculoskeletal pecularities of female puberty
- Lordosis /Swayback- Origin of many abdominal compression syndromes
- Bending of a straight vein compels its narrowing
- The lordogenetic midline congestion syndrome
- Neurological consequences of the midline congestion syndrome
- Successful treatment of a teenage girl who was unable to eat due to extreme postprandial pain and unable to walk due to spasticity in her left leg
- Severe ataxia in a young woman with severe spinal congestion – complete resolution after decompression of the left renal vein
- All compression syndromes are one: the spectrum of lordogenetic compressions
- Nutcracker-Syndrome is a misnomer! Lordogenetic left renal vein compression is a more appropriate name!
- May-Thurner-constellation (May-Thurner-syndrome, Cockett’s syndrome)
- Midline (congestion) syndrome
- Pelvic congestion syndrome
- Celiac Trunk Compression / Dunbar syndrome / MALS / Arcuate ligament syndrome
- Wilkie-Syndrome / Superior-mesenteric-artery-syndrome
- Compression of the vena cava inferior
- Evlauation of vascular compressions with the PixelFlux-method
- Connective tissue disorders predispose to multiple compressions
- Postural tachycardia syndrome (POTS) – the hemodynamic consequence of vascular compression syndromes and loose connective tissue
- Restless legs-a little known symptom of abdominal vascular compression syndromes
- Pudendal neuralgia in vascular compression syndromes
- A new sonographic sign of severe orthostatic venous pooling
- Migraine and Multiple Sclerosis
- Hemodynamic effect on cerebral perfusion in patients with multiple localised vascular compression.
- Treatment of vascular compression syndromes
- Fatal errors in the treatment of vascular compression syndromes
- Risks of stents in venous compression syndromes
- Surgical treatment of abdominal compression syndromes: The significance of hypermobility‐related disorders
- Nutcracker and May-Thurner syndrome: Decompression by extra venous tube grafting and significance of hypermobility related disorders
- Our surgical treatment of vascular compressions
- Chronic regional pain syndrome (CRPS) caused by venous compression and mechanical irritation of the coeliac plexus
- Vascular compression syndromes I recently detected
- Kaleidoscope of instructive cases
- Ultrasound Diagnostics
- Profile
- Functional colour Doppler ultrasound – how I do it
- Perfusion Measurement – PixelFlux-method
- Research
- Publications
- Nutcracker and May-Thurner syndrome: Decompression by extra venous tube grafting and significance of hypermobility related disorders
- Papers authored by Th. Scholbach
- Publications
- Inauguration of measurements of the tissue pulsatility index in renal transplants
- From nutcracker phenomenon to midline congestion syndrome and its treatment with aspirin
- First sonographic tissue perfusion measurement in renal transplants
- First sonographic bowel wall perfusion measurement in Crohn disease
- First sonographic renal tissue perfuison measurement
- First sonographic measurement of renal perfusion loss in diabetes mellitus
- PixelFlux measurements of renal tissue perfusion
- Why I prefer not to publish in journals but in the Internet
- Vessel stretching in nephroptosis – an important driver of complaints
- Publications
- Expertise
- Bornavirus Infection
- Scientific cooperation
- Cookie Policy
- Data protection
- Cookie Policy (EU)
- Impressum

Post-prandial pain in the right upper abdomen due to a newly detected compression syndrome of the right renal vein
Many patients suffer from unexplainable pain in the right upper abdomen or in the right upper back after a meal. I now detected a frequent reason for such complaints- a novel vascular compression syndrome.
In some patients the duodenal function is retarded or disturbed. Then , after the ingestion of food , the stomach empties large amounts of food into the duodenum. Now the descending portion of the duodenum progressively enlarges and exerts pressure onto the right renal vein. The vein is squeezed from above by the steadily distending duodenum and from below by the stiff right renal artery. The artery exerts a pulsatile pressure onto the right renal vein since the artery cannot move away because it lies on top of the lateral surface of the lumbar vertebra. This bony resistance with the artery on top presses the vein from below whereas the growing pressure from the distending duodenum presses the right renal vein from above. This causes a gradually increasing venous congestion of the right kidney which is felt as a growing pain in the right flank , in the right upper abdomen below the liver or in the right upper back.
I detected this condition in many patients in whom I meticulously observed the duodenal transport to rule out a Wilkie syndrome. The patients ingested tolerable amounts of food and fluid and then I started observing the transport in the descending and horizontal part of the duodenum.
In many patients an intermediate state exists resembling a low-grade Wilkie syndrome.
In other patients there is no narrowing of the passage between the aorta and the superior mesenteric artery, but an intrinsic deficiency of the duodenum and motor function does not allow a proper continuous transport of food from the pylorus across the descending portion of the duodenum and subsequently through the horizontal portion of the duodenum past the aortomesenteric fork.
These are relatively frequent conditions which do not fit in the pattern of a Wilkie syndrome and are often misdiagnosed as a gastroparesis. The gastroparesis is usually diagnosed with a scintigram showing a delayed emptying of the stomach. This is then interpreted as a decreased activity of the stomach. In fact, I never saw a decreased motor function of the stomach in these patients. To the contrary I often see a very hefty contraction of the stomach starting after the ingestion of food which is often accompanied by burping or the feeling of fullness or even gulping and sometimes vomiting.
So, despite the diagnosis of gastroparesis a strong peristaltic activity of the stomach presses food into the descending portion of the duodenum. Now the food distends the duodenum progressively exerting pressure onto the right renal vein according to the above-described mechanism. Then , only after multiple futile compressions, small amounts of food pass little by little across the aortomesenteric fork. In some patients the fork is relatively tight adding to the pressure in the contracting descending part of the duodenum. In other patients the fork is open but nevertheless a disturbed motor function of the descending part of the duodenum causes the above-described compression of the right renal vein.
In these relatively numerous patients with a disturbed contractile activity of the descending part of the duodenum and subsequent growing pain in the right upper abdomen I often could diagnose a Borna virus infection which is able to hamper a normal peristaltic activity of the duodenum and may be treated after a proper diagnosis with an anti-viral medication.
So, it is crucial to do a meticulous functional ultrasound examination to find the reason for post-prandial pain in the right upper quadrant which cannot be clarified by gastroscopy nor CT nor MRI imaging nor a conventional ultrasound examination.
It is necessary to prove the above-described mechanism by a pre–and post-prandial PixelFlux measurement of the blood flow in the right kidney which shows a deteriorating perfusion of the subcapsular vessels of the right kidney after a meal. This is the consequence of the growing venous counterpressure suppressing the blood flow in the tiny subcapsular vessels of the kidney when the pressure inside the right renal vein grows steadily after a meal.
Post-prandially increasing distension of the descending portion of the duodenum which exerts pressure onto the right renal vein. Then a jet-like emptying highlights the pressure but transports some amount of food across the aortomesenteric fork. In many patients multiple contraction waves are necessary to slightly diminish the pressure inside the steadily dilating duodenum. The increasing venous congestion explains pain in the right upper back (the position of the right kidney) and in the right upper quadrant (position of the painfully enlarging duodenum)

Side-by-side presentation of the relevant anatomic structures in a ultrasound image of the dilating descending duodenum squeezing the right renal vein
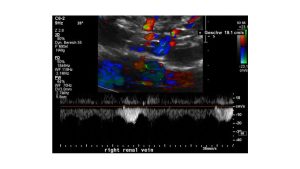
Direct visualisation of the pressure gradient exerted by the right renal artery onto the right renal vein during the compression of the right renal vein by the steadily enlarging duodenum from above after a meal. Here a slow venous flow before the compression within the renal hilum is demonstrated-19 cm/s.
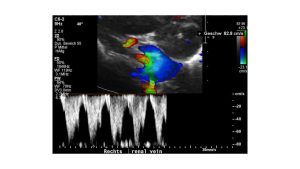
This image shows the pulsatile flow acceleration due to the compression of the right renal vein (blue vessel) by the compressing right renal artery (red vessel). The flow velocity increases to 81 cm/s! The flow is rhythmically interrupted due to the arterial pulse. The ensuing turbulences are highlighted by green pixels inside the blue vessel.
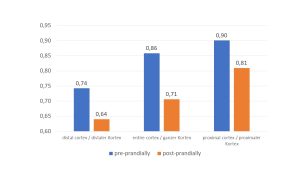
Ratio of the right/left renal perfusion in a PixelFlux measurement demonstrating the deteriorating right renal perfusion due to compression of the right renal vein by the post-prandially dilating duodenum and the right renal artery. The effect is most pronounced in the pressure sensitive subcapsular vessel in the distal cortex
