- Новые статьи
- Частная рактика для функциональной ультразвуковой диагностики для детей и взрослых
- Сосудистые явления сжатия
- Лечение сосудистых компрессионных синдромов
- Недавно открытые синдромы сдавления сосудов
- Калейдоскоп поучительных дел
- Ультразвуковая диагностика
- Услуги
- Функциональный цветной допплеровский ультразвук — как я это делаю
- Иссле́дование
- Квалификация
- Вирус болезни Борна (ВББ) или Борнавирус
- Научное сотрудничество
- Cookie Policy
- Cookie Policy (EU)

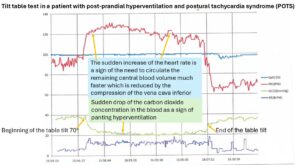
Patient with severe post-prandial hyperventilation and circulatory issues due to compression of the vena cava by the diaphragm and the down sliding liver
The patient is a 35-year-old female with a long history of postprandial issues. Among other symptoms, she was unable to eat sufficient amounts of food. Specifically, she avoided solid foods, which were less tolerated than fluids. One of the main symptoms was shortness of breath after a meal, which she felt was life-threatening, especially when she stood upright after eating, at which point she also experienced circulatory issues, such as dizziness and near fainting.
For over 10 years, conventional gastroenterological and cardiological diagnostics could not determine the cause of the problem.
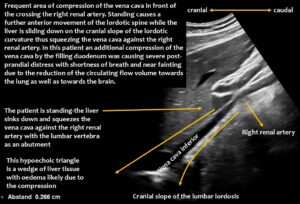
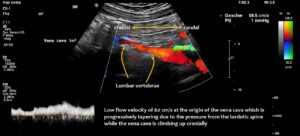
However, functional colour Doppler ultrasound revealed that the problems were caused by compression of the inferior vena cava. The patient’s increased lumbar lordosis, resulting from a connective tissue disorder (hypermobile Ehlers-Danlos syndrome), pushed the inferior vena cava ventrally.
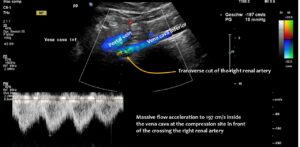
The upper lumbar vertebrae thus acted as a barrier against which the expanding duodenum pressed the vena cava. The situation was exacerbated by the duodenum not functioning properly, causing food to become lodged in the descending portion of the duodenum, directly in front of the inferior vena cava.
When the patient stood up, gravity pulled the liver downwards.
Due to the lax connective tissue, the liver was less fixed and thus developed orthostatic hepatoptosis, sliding down like a sled on a ramp — the cranial slope of the lumbar lordotic curvature — while standing. This compression was exacerbated by the perpendicular crossing of the right renal artery, which runs behind the vena cava and in front of the lumbar spine, acting as a bar and making the compression even more efficient.
Immediately after food was taken up, the stomach pumped it into the duodenum, which subsequently enlarged and compressed the vena cava.
This suddenly interrupted or massively compromised the venous return from the lower body hemisphere. This led to a sudden drop in the circulating blood volume. Due to reduced lung perfusion as a consequence of the reduction in central flow volume, panting developed to enhance oxygenation of the remaining small blood volume. At the same time, the reduced blood flow to the brain, in combination with hypocapnia as a result of hyperventilation to fight imminent compromise of oxygenation, caused dizziness and a sensation of near fainting.
Functional ultrasound can demonstrate the entire pathophysiological chain, from underlying lordosis to postprandial duodenal enlargement and subsequent vena cava compression, especially when standing after eating.
The logical treatments are reducing the lordosis, training the back muscles, and eventually decompressing the vena cava by wrapping it in a PTFE shield.