- New stuff to read and discuss
- What patients say
- Clinic / online appointments
- Why the diagnosis of a psychosomatic illness is often a misdiagnosis
- Vascular Compression Syndromes
- Do you have questions?
- Checklist vascular compression syndromes
- Description of your symptoms
- Researchers from the Mayo Clinic confirm my concept of the Midline Congestion Syndrome
- Explanation of gender-specific differences in the clinical symptoms of abdominal vascular compression syndromes: varicocele and penile/testicular pain – their main manifestation in men.
- Varicocoele is predominantly caused by left renal vein compression
- Musculoskeletal pecularities of female puberty
- Lordosis /Swayback- Origin of many abdominal compression syndromes
- Bending of a straight vein compels its narrowing
- The lordogenetic midline congestion syndrome
- Neurological consequences of the midline congestion syndrome
- Successful treatment of a teenage girl who was unable to eat due to extreme postprandial pain and unable to walk due to spasticity in her left leg
- Severe ataxia in a young woman with severe spinal congestion – complete resolution after decompression of the left renal vein
- All compression syndromes are one: the spectrum of lordogenetic compressions
- Nutcracker-Syndrome is a misnomer! Lordogenetic left renal vein compression is a more appropriate name!
- May-Thurner-constellation (May-Thurner-syndrome, Cockett’s syndrome)
- Midline (congestion) syndrome
- Pelvic congestion syndrome
- Celiac Trunk Compression / Dunbar syndrome / MALS / Arcuate ligament syndrome
- Wilkie-Syndrome / Superior-mesenteric-artery-syndrome
- Compression of the vena cava inferior
- Evlauation of vascular compressions with the PixelFlux-method
- Connective tissue disorders predispose to multiple compressions
- Postural tachycardia syndrome (POTS) – the hemodynamic consequence of vascular compression syndromes and loose connective tissue
- Restless legs-a little known symptom of abdominal vascular compression syndromes
- Pudendal neuralgia in vascular compression syndromes
- A new sonographic sign of severe orthostatic venous pooling
- Migraine and Multiple Sclerosis
- Hemodynamic effect on cerebral perfusion in patients with multiple localised vascular compression.
- Treatment of vascular compression syndromes
- Fatal errors in the treatment of vascular compression syndromes
- Risks of stents in venous compression syndromes
- Surgical treatment of abdominal compression syndromes: The significance of hypermobility‐related disorders
- Nutcracker and May-Thurner syndrome: Decompression by extra venous tube grafting and significance of hypermobility related disorders
- Our surgical treatment of vascular compressions
- Chronic regional pain syndrome (CRPS) caused by venous compression and mechanical irritation of the coeliac plexus
- Vascular compression syndromes I recently detected
- Kaleidoscope of instructive cases
- Ultrasound Diagnostics
- Profile
- Functional colour Doppler ultrasound – how I do it
- Perfusion Measurement – PixelFlux-method
- Research
- Publications
- Nutcracker and May-Thurner syndrome: Decompression by extra venous tube grafting and significance of hypermobility related disorders
- Papers authored by Th. Scholbach
- Publications
- Inauguration of measurements of the tissue pulsatility index in renal transplants
- From nutcracker phenomenon to midline congestion syndrome and its treatment with aspirin
- First sonographic tissue perfusion measurement in renal transplants
- First sonographic bowel wall perfusion measurement in Crohn disease
- First sonographic renal tissue perfuison measurement
- First sonographic measurement of renal perfusion loss in diabetes mellitus
- PixelFlux measurements of renal tissue perfusion
- Why I prefer not to publish in journals but in the Internet
- Vessel stretching in nephroptosis – an important driver of complaints
- Publications
- Expertise
- Bornavirus Infection
- Scientific cooperation
- Cookie Policy
- Data protection
- Cookie Policy (EU)
- Impressum

Genital pain on sitting – sometimes pudendal neuralgia – here long undetected subacute Bartholinitis along with Ehlers-Danlos syndrome and and multiple compression syndromes – diagnosis by PixelFlux
Medical history (June 2021)
The patient has been suffering since January 2020 from intolerable pain in the area of the labia majora on the left side, which increases unbearably when sitting, decreases from strength 8/10 to strength 5/10 when standing, and is felt about the same when walking. This pain is always present, except at night, and is felt as an internal swelling. In the meantime, the patient had complaints in the sense of cystitis, and was also able to empty the bladder only hesitantly in the morning. Now, however, micturition is painless and bladder emptying is possible without complications. Clinically, there is a hypermobile Ehlers-Danlos syndrome. Molecular genetics excluded all other forms of Ehlers-Danlos syndrome. The hyperextensibility of the connective tissue is expressed by the fact that the patient can press the thumb on the ipsilateral radius without any difficulty, can touch the floor with the palms when standing, the thumb sign and the little finger sign are positive.
When standing, the patient feels as if something like an internal prolapse is pushing down in the pelvis.
There was also a now repaired diaphragmatic hernia.
The pain in the genital area was also interpreted as coccygodynia. Infiltration of the region with a local anesthetic provided long-term relief but insufficient to allow undisturbed sedentary occupation.
In addition, there is left inguinal abdominal pain to a lesser degree at a level of 3/10 and under the left costal arch pain at a level of 2/10. The patient also reported left scapular pain and pain on the left side of the neck, sometimes accompanied by difficulty swallowing. Menstrual pain, respiratory problems, or swelling of the legs are denied. Food intake is not affected. Vomiting or diarrhea do not exist. Numerous medical consultations have not resulted in satisfactory improvement of her symptoms. Since May 21, there has been continuous vaginal bleeding, but no gynecological therapy has been initiated; the examination findings of the treating gynecologist were fine.
Clinical findings
Palpation and auscultation of the abdomen are unremarkable. There is no pathological resistance. On palpation of the perineum, however, a severe palpatory pain can be elicited at the dorsal commissure of the labia on the left side. Externally, there is questionable redness here, no swelling, no resistance. There is no vaginal secretion at present.
Sonographic findings
The urinary bladder is moderately full, sonographically unremarkable. The vagina is not swollen but is riddled with numerous small, dilated veins. The uterus is vigorous, anteflexed, and shows significant signs of pelvic congestion with dilated veins interspersing the myometrium in a spongy fashion, particularly prominent at the left circumference of the uterus. This pelvic congestion explains the left inguinal pain. In the internal iliac vein on the left, there is a slightly arterially modulated 667 ml/min of cranial outflow. On the right, 2 internal iliac veins are visible, which together drain 436 ml cranially. The perfusion on the left side is symmetrically increased to about double. The strong increase in perfusion on the left can be explained by the relief of the pelvic veins, which are increasingly dilated by gravity during standing, after the patient has moved to the supine position for examination and thus the influence of gravity on the pelvic congestion decreases. The congestion on the left can be explained as a result of the minor outflow obstruction via the arranged iliac vein communis at the promontory (see below).
The left common iliac vein has a flow velocity of 35 at the left flank of the os sacrum and a flow velocity of 89 cm/s at the junction with the right common iliac artery. However, a true luminal constriction is not visible at this crossing site. Rather, the flow acceleration arises from the arcuate course across the apex of the promontory.
In the supine position, a vena ovarica sinistra dilated to 8 mm can be visualized at the start of the examination. However, after repeated repositioning of the patient and assumption of a standing posture, the vessel collapses as the abdominal viscera descend into the pelvis. In this respect, pelvic congestion could be phasically fed by blood inflow from the left renal vein via an intermittently retrogradely perfused markedly dilated vena ovarica sinistra.
The vena cava is not compressed.
However, the patient’s pronounced lordosis lifts the aorta so far ventrally that there is almost complete compression of the left renal vein at the junction of the vessel over the arcuate branch of the renal artery. While in the left part of the renal vein the flow velocity is pulsatile modulated at 17 cm/s, flow velocities of up to 262 cm/s are found at the compression site in the supine position!
In the supine position, the flow volume in the abdominal aorta is 3659 ml/min, and the flow velocity in the aorta is 98 cm/s systolic.
The outlet of the truncus coeliacus is circumferentially compressed by the ligamentum arcuatum resulting in a flow acceleration to 201 cm/s in mid position of the diaphragm. In inspiration, this compression disappears, turbulent flow at the site of compression can no longer be detected, and flow velocity drops to 108 cm/s. Thus, there is a typical constellation of a ligamentum arcuatum syndrome, but without relevant clinical symptoms, except for the clinically suspected esophagitis.
The entire colonic frame is strongly meteoristically distended. When the intestines descend into the pelvis in the standing position, this leads to increasing pressure on the congested pelvic veins and to an increase in pelvic discomfort. In supine position the upper pole of the left kidney is 19.5, that of the right 17.4 cm cranial to the crista iliaca in standing position this distance decreases on the left side to 11.3, on the right side to 7.6 cm. Thus, there is a marked ptosis of both kidneys, consistent with Ehlers-Danlos syndrome, especially on the right. In standing, there is phasic relief of compression of the left renal vein, but this is short-lived. Flow velocities at the site of compression around 150 cm/s are then measured. In sitting, which is particularly difficult for the patient, the flow velocity increases again to 263 cm/s due to increasing compression of the left renal vein.
The hemodynamic relevance of renal vein compression is expressed by a markedly decreased volume perfusion of the left kidney in the PixelFlux measurement. This difference exists mainly in the supine position, where the perfusion of the left kidney is about 40% of that of the right kidney. In sitting and standing, the pronounced ptosis of the right kidney, less pronounced also on the left, causes a significant decrease in perfusion, especially on the right and a general reduction in renal perfusion. This contributes to increased blood flow into the pelvic circulation during sitting and standing, where it contributes to venous congestion.
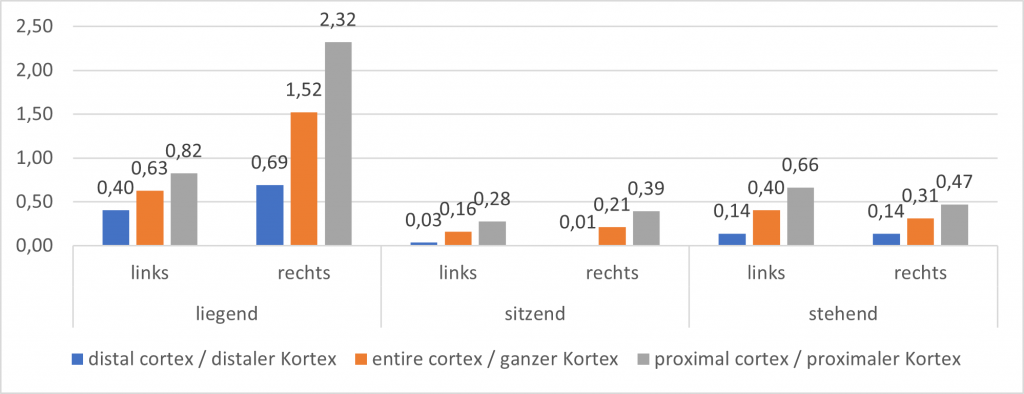
Parenchymal perfusion measurement of both kidneys using the PixelFlux technique Specification of perfusion intensity in [cm/s * cm²/cm²] as mean velocity of all color-coded pixels multiplied by the area of all color-coded pixels/the area of all pixels of the region of interest.
No sonographic changes characteristic of Crohn’s disease are found in the rectum or in other bowel segments.
The PixelFlux technique measures perfusion in the area of the left perineal inflammatory infiltrate. It is a multiple of the perfusion of the tissue on the right paravaginal side. From the sonographic point of view, this is a left bartholinitis. An appropriate antibiotic therapy was started.
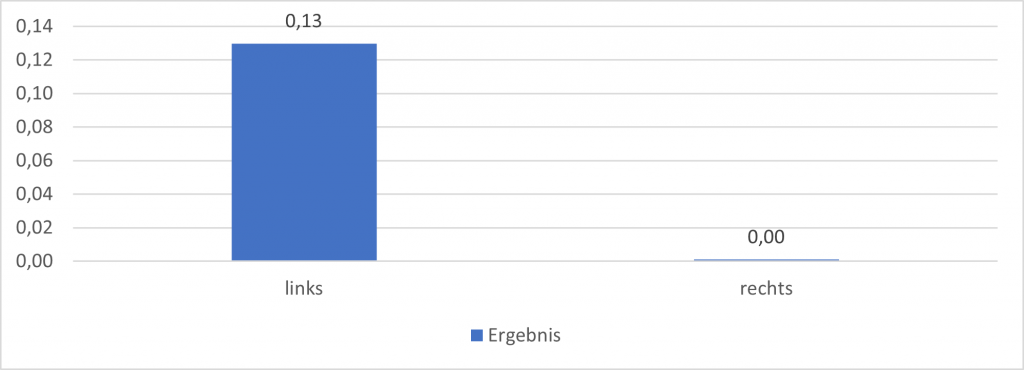
Parenchymal perfusion measurement Labia maiora with the PixelFlux technique Specification of the perfusion intensity in [cm/s * cm²/cm²] as the mean velocity of all color-coded pixels multiplied by the area of all color-coded pixels/the area of all pixels of the region of interest.
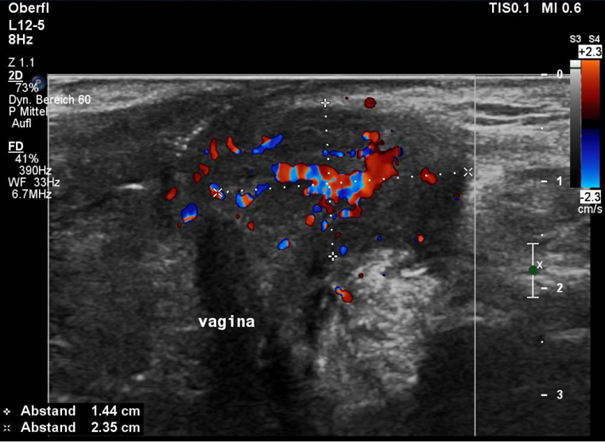
Transverse color Doppler ultrasound of the vulva at the dorsal commissure of the labia majora. On the left side, there is a well-demarcated, hyperperfused inflammatory infiltration at the site of Bartholin’s gland, exactly where the pain was localized by 1-finger palpation.
Differentially considered left pudendal nerve neuralgia is illuminated by examining the ischium from medial and the area of Alcock’s canal. No venous congestion signs in the area of the pudendal nerve and Alcock’s canal can be seen. Rather, the pointum maximum of the pain is clearly medial to the pudendal nerve at the dorsal commissure of the greater labia on the left.
Diagnoses
- Bartholinitis on the left side-antibiotic therapy with 2 x 500 mg cefuroxime was initiated
- pelvic congestion with feeding of renal vein blood (intermittent) via the vena ovarica sinistra, but mainly due to the clinical
- hypermobile Ehlers-Danlos syndrome.
- low-grade flow obstruction of the left common iliac vein due to the arcuate course of the vessel over the raised promontory
- clinically almost inapparent Median arcuate ligament syndrome
- massive lordogenetic renal vein compression on the left side, insufficiently compensated by collaterals
- pronounced ptosis of both kidneys, right more than left
- High-grade perfusion reduction especially of the right kidney in standing position with consecutive increase of hyperperfusion of the pelvic organs
*** Translated with www.DeepL.com/Translator (free version) ***
