- New stuff to read and discuss
- What patients say
- Clinic / online appointments
- Why the diagnosis of a psychosomatic illness is often a misdiagnosis
- Vascular Compression Syndromes
- Do you have questions?
- Checklist vascular compression syndromes
- Description of your symptoms
- Researchers from the Mayo Clinic confirm my concept of the Midline Congestion Syndrome
- Explanation of gender-specific differences in the clinical symptoms of abdominal vascular compression syndromes: varicocele and penile/testicular pain – their main manifestation in men.
- Varicocoele is predominantly caused by left renal vein compression
- Musculoskeletal pecularities of female puberty
- Lordosis /Swayback- Origin of many abdominal compression syndromes
- Bending of a straight vein compels its narrowing
- The lordogenetic midline congestion syndrome
- Neurological consequences of the midline congestion syndrome
- Successful treatment of a teenage girl who was unable to eat due to extreme postprandial pain and unable to walk due to spasticity in her left leg
- Severe ataxia in a young woman with severe spinal congestion – complete resolution after decompression of the left renal vein
- All compression syndromes are one: the spectrum of lordogenetic compressions
- Nutcracker-Syndrome is a misnomer! Lordogenetic left renal vein compression is a more appropriate name!
- May-Thurner-constellation (May-Thurner-syndrome, Cockett’s syndrome)
- Midline (congestion) syndrome
- Pelvic congestion syndrome
- Celiac Trunk Compression / Dunbar syndrome / MALS / Arcuate ligament syndrome
- Wilkie-Syndrome / Superior-mesenteric-artery-syndrome
- Compression of the vena cava inferior
- Evlauation of vascular compressions with the PixelFlux-method
- Connective tissue disorders predispose to multiple compressions
- Postural tachycardia syndrome (POTS) – the hemodynamic consequence of vascular compression syndromes and loose connective tissue
- Restless legs-a little known symptom of abdominal vascular compression syndromes
- Pudendal neuralgia in vascular compression syndromes
- A new sonographic sign of severe orthostatic venous pooling
- Migraine and Multiple Sclerosis
- Hemodynamic effect on cerebral perfusion in patients with multiple localised vascular compression.
- Treatment of vascular compression syndromes
- Fatal errors in the treatment of vascular compression syndromes
- Risks of stents in venous compression syndromes
- Surgical treatment of abdominal compression syndromes: The significance of hypermobility‐related disorders
- Nutcracker and May-Thurner syndrome: Decompression by extra venous tube grafting and significance of hypermobility related disorders
- Our surgical treatment of vascular compressions
- Chronic regional pain syndrome (CRPS) caused by venous compression and mechanical irritation of the coeliac plexus
- Vascular compression syndromes I recently detected
- Kaleidoscope of instructive cases
- Ultrasound Diagnostics
- Profile
- Functional colour Doppler ultrasound – how I do it
- Perfusion Measurement – PixelFlux-method
- Research
- Publications
- Nutcracker and May-Thurner syndrome: Decompression by extra venous tube grafting and significance of hypermobility related disorders
- Papers authored by Th. Scholbach
- Publications
- Inauguration of measurements of the tissue pulsatility index in renal transplants
- From nutcracker phenomenon to midline congestion syndrome and its treatment with aspirin
- First sonographic tissue perfusion measurement in renal transplants
- First sonographic bowel wall perfusion measurement in Crohn disease
- First sonographic renal tissue perfuison measurement
- First sonographic measurement of renal perfusion loss in diabetes mellitus
- PixelFlux measurements of renal tissue perfusion
- Why I prefer not to publish in journals but in the Internet
- Vessel stretching in nephroptosis – an important driver of complaints
- Publications
- Expertise
- Bornavirus Infection
- Scientific cooperation
- Cookie Policy
- Data protection
- Cookie Policy (EU)
- Impressum

Diaphragmatic compression of the hepatic veins
Here I describe a novel compression syndrome which I detected recently in a number of patients-the variable compression of the hepatic veins by the diaphragm during respiration.
Within the last year I saw multiple patients with complaints in the right upper abdomen-pain , tension, fullness related to this diaphragmatic hepatic vein compression .
In these patients I saw a venous outflow obstruction from the liver which in some of the patients’ caused and intermittent swelling of the liver which may be the reason for the above-mentioned complaints.
An outflow obstruction of the hepatic veins at their confluence into the vena cava inferior your is a well known entity called Budd-Chiari syndrome. This is usually caused by a thrombotic obstruction of this confluence or by fibrous ligaments or membranes which are thought to stem from the embryonic development of these veins and rarely due to other reasons.
So far unknown yet is a compression of these veins by the diaphragm which I detected in a number of patients by means of functional colour Doppler ultrasound.
In these patients turbulences are found at the confluence of the hepatic veins directly in front of their entrance into the vena cava inferior. These turbulences are caused by a narrowing of the hepatic veins producing an accelerated flow. This is a general sonographic hallmark of a Budd-Chiari syndrome.
In contrast to known pathologies producing a Budd-Chiari syndrome in the patient’s I observed this constriction of the hepatic veins was not constant but respiratory dependent. The degree of the constriction varied with inspiration and expiration. With this respect this newly detected compression syndrome resembles the median arcuate ligament syndrome.
In the median arcuate ligament syndrome (MALS) the aortic hiatus compresses the coeliac plexus and trunk from above by means of the sharp median arcuate ligament bridging the left and right diaphragmatic crus.
In the diaphragmatic compression of the hepatic veins mechanism is very similar. The passage of the vena cava from the abdominal cavity into the thorax is possible due to an opening in the diaphragm which resembles the aortic hiatus.
In some patients the movement of the diaphragm from its inspiratory to its expiration position cuts into the confluence of the hepatic veins. This produces a variable narrowing of this confluence with a subsequent turbulent flow acceleration and venous congestion of the liver. Depending on the degree and duration of this compression a venous outflow obstruction of the liver a result producing a swelling of the liver (hepatomegaly) with ensuing pain in the right upper abdomen, tenderness and fullness.
Normal blood flow within the central portion of the middle hepatic vein inside the liver with a maximum flow velocity of 34 cm/s.
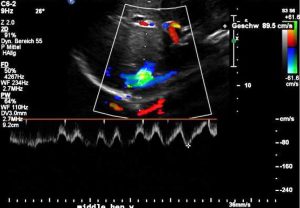
Significantly accelerated blood flow within the middle hepatic vein at the confluence with the vena cava inferior resulting in a turbulent flow acceleration (green pixels) and a maximum flow velocity of 89 cm/s.
Sharp reduction of the flow velocity within the middle hepatic vein at the confluence during inspiration with a flow velocity dropping to 49 cm/s.
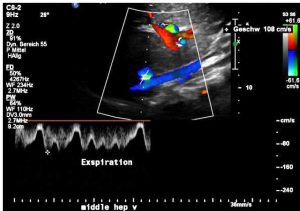
In expiration due to the compression of the confluence of the hepatic veins the flow suddenly accelerates to 108 cm/s.