- Nouveaux articles
- Cabinet médical / Prise de rendez-vous en ligne
- Syndrome de compression vasculaire
- Avez-vous des questions ?
- Liste de contrôle des syndromes de compression vasculaire
- Constellation de May-Thurner / Cockett’s syndrome
- Syndrome de la ligne médiane
- Syndrome de congestion pelvienne
- Syndrome de compression du tronc coeliaque – Syndrome de Dunbar – Syndrome du ligament arqué médian – MALS
- Syndrome de Wilkie / syndrome de l’artère mésentérique supérieure
- Compression de la veine cave inférieure
- Névralgie pudendale dans les syndromes de compression vasculaire
- Traitement des syndromes de compression vasculaire
- Syndromes de compression vasculaire I récemment détectés
- Un kaléidoscope de cas instructifs
- Diagnostic ultrasons
- L’échographie Doppler couleur fonctionnelle – comment je m’y prends
- Qualifications, expériences et compétences
- Collaboration scientifique
- Cookie Policy
- Cookie Policy (EU)
- Impressum

4-D volume flow measurements of the jugular veins reveal the origin of extreme positional headaches
4-D volume flow measurements of the jugular veins reveal the origin of extreme positional headaches in a patient with abdominal, pelvic and cervical venous compression syndromes
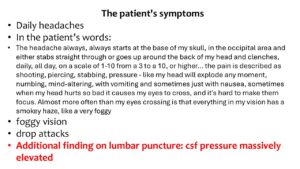
This is a 36-year-old female patient with hypermobile Ehlers-Danlos syndrome (hEDS) and extreme positional headaches, which can be explained by functional, qualitative and four-dimensional ultrasound. The headaches are a consequence of the pressurisation of the skull.
The increased intracranial pressure caused debilitating headaches and disturbed vision.
These headaches changed with body and head posture.
The cause was compression of the left renal vein, the left common iliac vein, both jugular veins and the left cephalic vein.
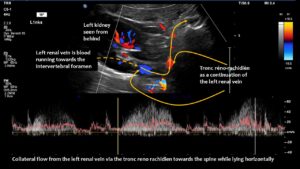
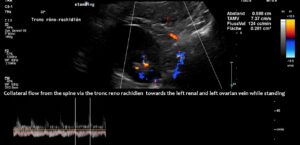
The main driving force was the compression of the left renal vein, as this vein transports most of the blood in the lower body hemisphere. Compression of this vein forces blood to run down the left ovarian vein towards the left internal and common iliac veins. The blood then tries to cross the spine to reach the inferior vena cava. This vessel returns blood to the heart. However, in this patient, the left common iliac vein was also compressed. Consequently, the increased pressure in the left renal vein could only be relieved by creating an additional collateral pathway. This connects the left renal vein with the spinal canal and is called tronc réno-rachidièn .
Large volumes of blood from the left renal vein enter the spinal canal and run along the spinal veins (epidural plexus) towards the skull, entering the intracranial sinuses. They can then leave the skull via the vertebral veins, but mainly via the jugular veins.
The vertebral veins are not helpful in this process, as they run inside bony rings along the cervical vertebrae. These bony rings prevent these veins from enlarging, which would be necessary to take up the additional blood from the skull.
Therefore, the jugular veins are the main escape route for the additional blood from the skull that stems from the left renal vein.
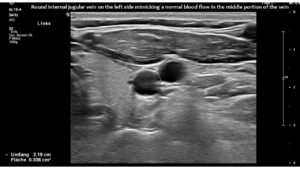
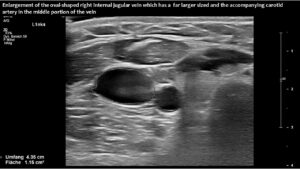
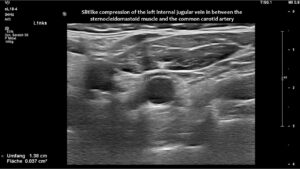
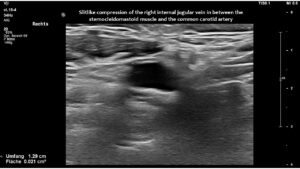
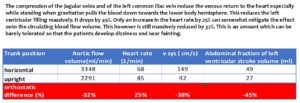
However, in this patient, both jugular veins were compressed. The middle portion of the internal jugular vein was pushed ventrally by the increased cervical lordosis on both sides, becoming squeezed between the carotid artery and the sternocleidomastoid muscle.
Increased cervical lordosis is a very common feature in patients with EDS. This increased curvature is necessary for compensating for the increased lumbar lordosis and thoracic kyphosis in these patients.
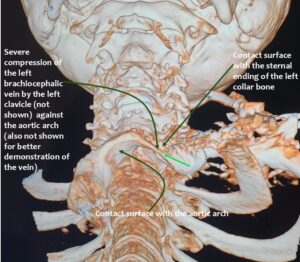
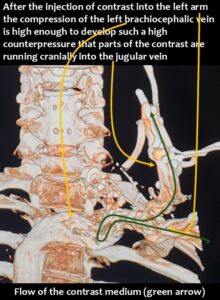
In addition, the patient had compression of the left brachiocephalic vein.
Consequently, blood had difficulty leaving the skull, resulting in continuously increased pressure and severe headaches, as well as other neurological dysfunction. The left side was more affected due to the double compression. This was clearly demonstrated by four-dimensional volume flow measurements in both jugular veins.
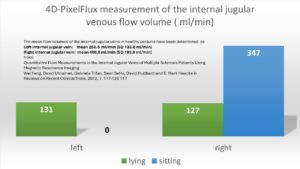 Only a four-dimensional volume flow measurement of the jugular veins can determine the cause of the daily headaches. The overall reduction in venous outflow from the brain in both jugular veins, totalling 258 mL/min, is significantly lower than the normal average volume of 719 mL/min. Consequently, the patient can eliminate only 36% of the required flow volume, while additional volume is forced into the skull from the left renal vein via the tronc réno-rachidien and from the left common iliac vein via the left ascending lumbar vein. This results in a chronic increase in intracranial pressure, as demonstrated by the elevated cerebrospinal fluid pressure obtained through a lumbar puncture. When the left jugular vein is also completely compressed due to increasing cervical lordosis when upright, the headaches become unbearable, accompanied by additional neurological symptoms as described by the patient.
Only a four-dimensional volume flow measurement of the jugular veins can determine the cause of the daily headaches. The overall reduction in venous outflow from the brain in both jugular veins, totalling 258 mL/min, is significantly lower than the normal average volume of 719 mL/min. Consequently, the patient can eliminate only 36% of the required flow volume, while additional volume is forced into the skull from the left renal vein via the tronc réno-rachidien and from the left common iliac vein via the left ascending lumbar vein. This results in a chronic increase in intracranial pressure, as demonstrated by the elevated cerebrospinal fluid pressure obtained through a lumbar puncture. When the left jugular vein is also completely compressed due to increasing cervical lordosis when upright, the headaches become unbearable, accompanied by additional neurological symptoms as described by the patient.
Without this sophisticated technique, it would be unclear how severe the pressurization of the skull was and that, despite compression of both jugular veins, the right one was the main escape route from the skull.
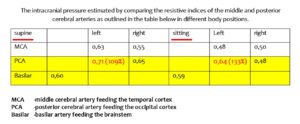
Measuring transcranial flow velocity in the intracranial arteries could provide evidence of localised brain pressurisation effects by demonstrating increased vascular resistance in the left posterior cerebral artery while sitting. This artery supplies the visual cortex. The patient suffered from severe visual disturbances.
This occurred when the patient experienced more severe headaches. This was because the outflow from the left jugular vein was completely blocked as soon as the patient sat up, affecting the left posterior cerebral artery. This could only be demonstrated using 4D volume flow measurements of both jugular veins in different patient positions.