- Praktyka medyczna
- Zespoły ucisku naczyniowego
- Czy masz jakieś pytania?
- Lista kontrolna Syndromy ucisku naczyniowego
- Charakterystyka układu mięśniowo-szkieletowego dojrzewania płci żeńskiej
- Lordozy / wydrążone plecy – Przyczyna licznych zespołów ucisku brzucha
- Zespół „dziadka do orzechów” jest błędną nazwą
- Zespół Midline (przeciążenie narządów linii środkowej)
- Zespół przeciążenia miednicy (przeciążenie organów miednicowych)
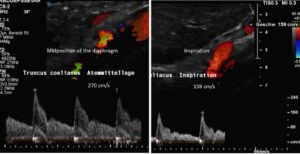
- Truncus coeliacus compression / Dunbar syndrome / MALS / Ligamentum arcuatum syndrome
- Zespół Wilkiego / zespół mezentryczny (arteria mesenterica superior)
- Kwantyfikacja zespołów ucisku naczyniowego przy użyciu techniki PixelFlux
- Neuralgia nadbrzusza w zespołach kompresji naczyniowej
- Leczenie zespołów ucisku naczyniowego
- Niedawno odkryte zespoły ucisku naczyniowego
- Funkcjonalne kolorowe ultradźwięki dopplerowskie – jak ja to robię
- Durchblutungsmessung – PixelFlux-Verfahren
- Badania
- Ekspertyza
- Zakażenie wirusem Bornavirusa
- Współpraca naukowa
- Cookie Policy
- Cookie Policy (EU)

A patient with chronic regional pain syndrome (CRPS) – successfully treated by venous decompression
CRPS is a poorly understood condition. Those affected suffer from pain, hyperaesthesia, swelling and immobilisation of their extremities. Not all cases of CRPS are preceded by trauma.
It is thought that the swelling and pain are a consequence of disturbed perfusion and stimulation of the sympathetic nervous system.
Patients are often unable to use their hands and feet, which can lead to immobilisation. In the late stages of the disorder, muscle wasting and joint contracture may occur.
The overall prognosis for those affected is poor.
Treatment is limited to physiotherapy, painkillers, and blocking the sympathetic nervous plexuses. Typically, only the progression of the disease is halted, and a cure is rarely achieved. There are cases of spontaneous resolution of symptoms. The reason for this is also unknown.
Case report of a patient with successfully treated CRPS
I had the opportunity to diagnose a female patient with CRPS. Four years ago, she experienced spontaneous pain and swelling in her left foot. Initially, the swelling persisted for several days and was followed by severe pain and bluish discolouration of the foot. It was at this time that the diagnosis of CRPS was established.
At the time of presentation, she was unable to walk unaided for more than a few steps and experienced severe restrictions in her ability to work. Standing upright increased the swelling of her foot and, later, her entire left leg. An upright position also provoked a bluish discolouration. Furthermore, she reported a circumscribed feeling of tension around the left knee joint.
Sonographic findings:
- A compression of the popliteal vein
- A compression of the left common iliac vein
- A compression of the left renal vein flooding the pelvic veins by collaterals
- A compression of the vena cava.
- In addition the patient was suffering from an increased sympathetic tone by a compression of the coeliac ganglion as a consequence of the compression of the coeliac trunk.
The pain anmd swelling below her left knee was caused by a combination of multiple venous compression syndromes which prevented a normal drainage of the affected left leg thus causing a chronic regional pain syndrome (CRPS).
Here the complete compression of her popliteal vein is demonstrated when she fully straightened her knee. Only after flexing her knees to an angle of 30° was her peripetal venous perfusion reinstated.
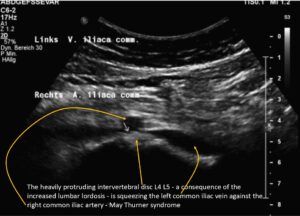
Further upstream the next outflow obstruction from the left leg is a May-Thurner syndrome due to a severe compression of the left common iliac vein:
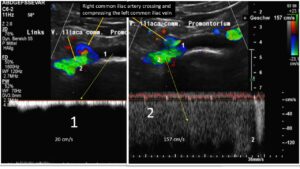 The subsequent congestion of the pelvic circulation was massively aggravated by a left renal vein compression which pours large amounts of blood towards the pelvic circulation via its collaterals-mainly the left ovarian vein. Due to the obstruction of the pelvic outflow the additional large left renal collateral flow volume is massively affecting the outflow from the left leg thus fuelling the chronic regional pain syndrome there.
The subsequent congestion of the pelvic circulation was massively aggravated by a left renal vein compression which pours large amounts of blood towards the pelvic circulation via its collaterals-mainly the left ovarian vein. Due to the obstruction of the pelvic outflow the additional large left renal collateral flow volume is massively affecting the outflow from the left leg thus fuelling the chronic regional pain syndrome there.
The severe congestion of the left kidney is highlighted by PixelFlux measurements of the renal parenchyma of both kidneys, as shown in the diagram below. There is severe suppression of parenchymal perfusion, which is most evident in the small subcapsular vessels (blue columns), the most pressure-sensitive vessels in the kidney. Here, a reduction in volume flow of 30% compared to the right kidney is evident.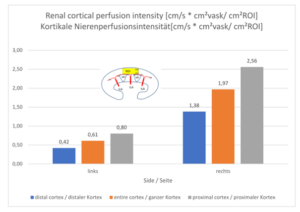
The exaggerated lumbar lordosis was compressing the inferior vena cava, which increased the backflow pressure in the left leg.
The chronic regional pain syndrome component was fuelled by activation of the sympathetic nervous system, resulting from compression of the largest sympathetic nerve plexus: the celiac plexus. In this patient, the coeliac plexus was severely compressed by a tightly straddling median arcuate ligament at the origin of the coeliac trunk. This is another consequence of increased lumbar lordosis, which pulls the arch formed by the two diaphragmatic crus legs tight.
The patient underwent surgery to reduce compression of the abdominal veins and coeliac plexus, resulting in prompt resolution of swelling in her left leg, hyperaesthesia and pain, and gradual restoration of mobility.
Only 4 weeks after the operation the patient wrote:
„Dear Prof. Scholbach, It has now been over a month since Prof. Sandmann performed the operation, and I am pleased to report that I am doing very well.
My left foot has developed wonderfully, so that I can already walk a few metres without crutches. My gait is still a little uneven and stiff, of course, but that will improve with consistent physiotherapy and exercises at home. True to the motto ‘practice makes perfect’. My foot is not sensitive to touch and can tolerate cold, heat, water and wind or draughts, so I can relax in a room with the window open. The swelling has also gone down considerably. I can even wear normal shoes for a certain amount of time. So my life is completely different from before….Dr —from Pain Therapy Centre, my pain therapist Dr … and all my other therapists are absolutely thrilled with the results of the operation. My pain therapist even said that I was a medical sensation….”
Six years after the operation, the patient can still move around smoothly and painlessly, which is a great success.
Explanation of the treatment success:
The rationale behind the treatment was to alleviate the joint effects of multiple venous compressions affecting the drainage of the left leg and chronic irritation of the largest sympathetic nervous plexus: the coeliac plexus.
In arcuate ligament syndrome, the coeliac plexus is compressed between the lower margin of the aortic hiatus and the coeliac artery. This results in persistent mechanical activation of this large sympathetic nervous network.
It was understood that sympathetic activation produced arterial hyperperfusion of the affected limb, as well as multiple obstructions to venous drainage, both of which contributed to swelling, pain, discolouration, and hypersensitivity in the left leg.
Thus, decompressing the coeliac plexus and improving drainage from the left leg restored normal perfusion and vegetative innervation to the blood vessels in regions affected by CRPS.