- Neue Artikel
- Was Patienten sagen – Fortsetzung
- Praktiken/bokning av möten online
- Gefäßkompressionssyndrome
- Haben Sie Fragen?
- Checkliste Gefäßkompressionssyndrome
- Muskuloskelettale Besonderheiten der weiblichen Pubertät
- Lordose /Hohlkreuz – Ursache zahlreicher abdomineller Kompressionssyndrome
- Das ”Nussknacker”-Syndrom ist eine Fehlbezeichnung
- May-Thurner-Konstellation /May-Thurner-Syndrom/Cockett’s syndrome/Vena iliaca-Kompressionssyndrom
- Mittelliniensyndrom (Stauung der Mittellinienorgane)
- Pelvines Kongestionssyndrom
- Truncus-coeliacus-Kompression / Dunbar-Syndrom / MALS / Ligamentum arcuatum-Syndrom
- Wilkie-Syndrom / Arteria-mesenterica-superior-Syndrom
- Quantifizierung der Gefäßkompressionssyndrome mit der PixelFlux-Technik
- Bindegewebserkrankungen begünstigen kombinierte Kompressionssyndrome
- Pudendusneuralgie bei vaskulären Kompressionssyndromen
- Migräne und Multiple Sklerose
- Behandlung von Kompressionssyndromen
- Vaskulära kompressionssyndrom som jag nyligen upptäckt
- Kaleidoskop lehrreicher Krankheitsverläufe
- Ultraschalldiagnostik
- Leistungsspektrum
- Funktioneller Farbdoppler-Ultraschall – wie ich ihn verstehe
- Durchblutungsmessung – PixelFlux-Verfahren
- Forschung
- Publikationen
- Artiklar författade av Th. Scholbach
- Eigene Publikationen
- Erstbeschreibung der Bestimmung des Gewebsperfusionsindexes in Nierentranplantaten
- Erstbeschreibung des Mittellininesyndroms – Aspirintherapie
- Erste sonografische Gewebsperfusionsmessung in Nierentransplantaten
- Erste sonografische Tumorperfusionmessung und Korrelation zur Tumoroxygenierung
- Erstmalige Darmwandperfusionsmessung bei M. Crohn
- Erstmalige sonografische Gewebsperfusionmessung der Nieren
- Erstmaliger Nachweis von Frühveränderungen der Nierenperfusion bei Diabetes mellitus
- PixelFluxmessung der Nierengewebsperfusion
- Publikationen
- Expertise
- Bornavirusinfektion
- Wissenschaftliche Zusammenarbeit
- Cookie-Richtlinie
- Hinweise zu medizinischen Erläuterungen
- Datenschutzerklärung
- Cookie Policy (EU)

Enigma resolved: vomiting during hip stretching
Headaches and vomiting while standing upright and lying supine – improvement only after crossing the legs with external rotation of the hip
(intraoperative images by courtesy of Professor Wilhelm Sandmann)
Summary
The patient suffered from multiple vascular compression syndromes which completely explained her symptoms. The most enigmatic symptom was the strict dependency of her headaches and congestion of the shoulders, arms and neck as well as the vomiting from the position of her right leg. Flexing and external rotation of the right hip promptly relieved or the above-mentioned ailments.
The reason for this very strange constellation was the variable perfusion of the epidural plexus which was fed by a strong tronc réno-rachidièn. The perfusion of the tronc réno-rachidièn was strictly dependent on the actual degree of her lumbar lordosis. Thus, reducing the lumbar lordosis by flexing the hips reduced the perfusion of the tronc réno-rachidièn and thereby decreased the intraspinal pressure. The intraspinal pressure was immediately transferred towards the skull. Increasing intraspinal and intracranial pressure could be demonstrated by changing perfusion of the middle cerebral artery in the patient. Thus, simultaneous measurements of the volume of the collateral circulation towards the spinal canal, measurement of the intracranial perfusion as a substitute for the intracranial pressure and renal parenchymal perfusion under different positions of the hip proved the causal relationship of hip external rotation/flexion and increasing congestion of the upper parts of the body/increasing intracranial pressure due to the left renal venous congestion and the varying compression of the left common iliac vein.
Medical history
The actual medical history of the 39 year old lady, mother of a 4 year old son, started in April 2019 after a suspected first miscarriage within the fourth gestational week. Then she developed a weakness of both legs, predominantly on the left side and moderate pelvic pain. In August last year a second miscarriage occurred in the third week and the pain in the pelvis increased but spontaneously resolved.
In November 2019 an antiphospholipid syndrome was diagnosed, the patient had a third miscarriage in the fourth week and increasing radicular left and right leg pain with severe weakness of the muscles from segment S 1 and 2. At that time a steroid treatment improved weakness and pain in the legs.
In April 2000, a 4th miscarriage occurred, and nausea, lightheadedness and hypotension developed- steroids did not help anymore. In May 2020, a Tarlov cyst was aspirated under CT guidance but to no avail.
Then, in July 2020 a pelvic congestion syndrome was diagnosed, and a nutcracker syndrome was suspected. One month later a first partial embolization of the left ovarian vein was started to reduce the pelvic congestion. After a short improvement, the symptoms reoccurred and increased. Then unfortunately, after a second embolization of the left renal vein, a lung embolism occurred with subsequent decreased oxygenation. All the deep pelvic pain resolved when the patient assumed a quadruped position.
An Ehlers-Danlos syndrome was suspected but not diagnosed by molecular diagnostics. Moreover, Marfanoid features are evident. In 2013 a thrombosis of the femoral vein occurred, but no clotting diagnosis was started yet.
Actually, the most annoying symptom is that the patient cannot stand for more than 5 minutes. Then she develops nausea, lightheadedness, severe pain and vomiting and can find relieve only while lying down and flexing her hips and rotating them externally. The pain in the pelvic region is now a constant one with a severity of 6/10 but sometimes increases to 9/10. The corticoid treatment does not help anymore with this pain. Nausea is accompanied by bloating and a tendency of fainting. Sometimes the patient observes urinary retention and vomits regularly with an average frequency of 1/week. Another important observation is that also the intake of large amounts of fluid increases her nausea. So, the patient is also not able to lie flat on her back and uses 4 pillows to keep her head and thorax in an elevated position to prevent nausea. Diuretics help to reduce the nausea. Hematuria has been ruled out and the glomerular filtration rate is in the lower normal range. After the second embolization which unfortunately caused lung embolism relevant episodes of a reduced lung function still occur.
The patient did not lose weight. Her actual weight is 60 kg. In the last months she lost some weight, but she tried to eat enough to gain weight again. Her height is 174 cm which is exceptional for her ethnicity. The patient explains this with her marfanoid constitution.
Clinical findings
The abdominal palpation reveals tenderness in the groin region on both sides. The abdominal auscultation does not find a disturbed peristalsis or vascular bruits. No abdominal lump is palpable. The subcutaneous vessels on both thighs and the abdominal ones are non-dilated.
Sonographic findings
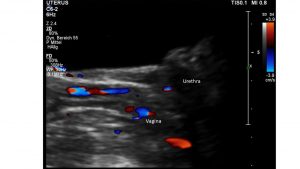
At the beginning of the examination the urinary bladder is well filled and unremarkable with respect to its wall and its content. Nevertheless, there are enlarged veins surrounding the urethra, the vagina, and the distal rectum.
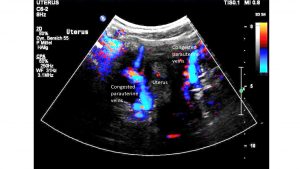
Moreover, enlarged veins are found within the walls of the urethra, the vagina, and the rectum but also and even more pronounced within and around the uterus.
This constitutes a severe pelvic congestion. There is no free abdominal fluid.
The blood flow within the left internal iliac vein is reduced and in the right internal iliac vein a changing flow direction is detected. This changing flow direction is caused by a variable compression of the cephalad portion of the right common iliac vein at the entrance to the pelvis. Here, due to the severe anterior inclination of the entire pelvis, the vein is compressed by the fifth lumbar vertebra from behind and by a small bowel loop in front of the vein. This compression by the bowel is made easy due to the severe uplifting of the lumbar spine with a minimum distance to the inner lining of the abdominal wall of only 8 mm. Thus, it is easy for bowel loops to add sufficient pressure onto the pre-compressed segment of the right common iliac vein to produce a reflux into the right internal iliac vein. The details of the volume flow in all abdominal veins is given in a table at the end of this report.
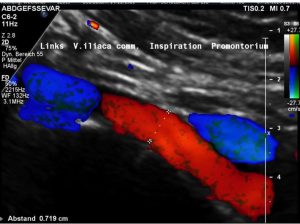
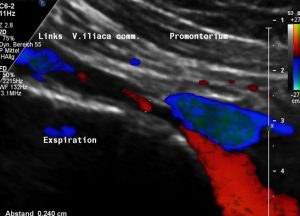
The pelvic congestion and the disturbed drainage of the left common iliac vein can be explained by a May-Thurner constellation. The left common iliac vein is compressed underneath the right common iliac artery thus producing a variable flow acceleration (see table). 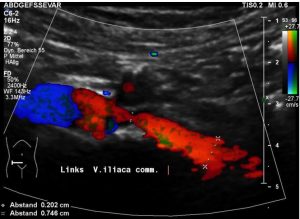 In inspiration the reduced intrathoracic pressure drags sufficient volumes from the pelvic circulation across the compression site thus opening the compression for short intervals.
In inspiration the reduced intrathoracic pressure drags sufficient volumes from the pelvic circulation across the compression site thus opening the compression for short intervals.
Most of the time the vein is collapsed or compressed by the right common iliac artery.
Thus, most of the time a substantial flow acceleration is found (see table and images).
A severe lumbar lordosis reduces the distance between the spine and the abdominal wall to 8 mm only:
The vena cava runs along the lordotic spine but is not compressed. There is a normal portal vein perfusion and a normal perfusion of the hepatic veins at their entrance to the vena cava. No thrombosis within the vena cava inferior and no thrombosis within the vena cava superior can be detected.
The jugular vein on the right side shows some narrowing and substantial flow acceleration which is not influenced by the intake of fluid or the position of the hips.
The left renal vein is completely compressed while crossing the aorta.
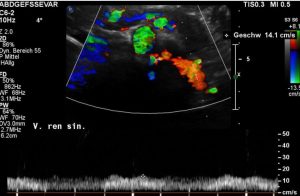
Complete compression of the left renal vein – red signal – between the aorta – large green circle – and the superior mesentric artery – small grteen circle.
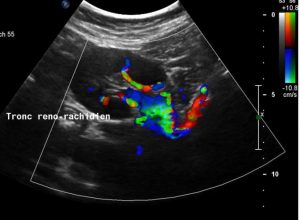
The entire blood of the left kidney is circumvented via a Tronc reno-rachidièn towards the hemi-azygos vein and the epidural plexus.
The flow volume within this collateral perfusion changes within seconds after the intake of oral fluid (400 mL plain water) and after flexing or stretching the hips with internal or external rotation. Simultaneously, the nausea and an impulse to vomit is produced at the same time as a substantial increase of the perfusion of the Tronc reno-rachidièn can be measured. The details and the timeline of this development is further given in a separate diagram at the end of this report. Fluid intake produces an increased blood flow in the left compared to the right kidney which is not followed by nausea and vomiting as long as the drainage via the Tronc reno-rachidièn does not exceed about 700 ml/min.
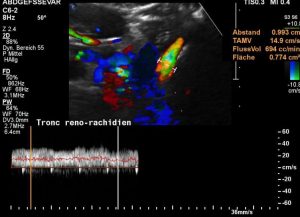
Reliable blood volume flow measurement inside the tronc réno-rachidièn to evaluate the congestion of the spinal canal
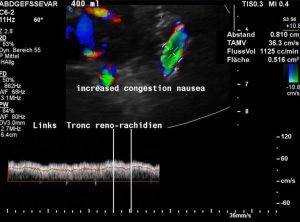
Increasing congestion of the spinal canal during stretching of the hips – simultaneous vomiting, headache, nausea and unbearable abdominal pain develop
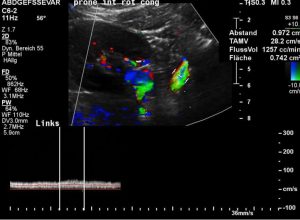
Maximum congestion of teh epidural plexus inside the spinal canal – pressure is transferred to the brain by the cerebrospinal fluid
A further increase of the collateral flow above about 900 ml/min is followed by nausea and a simultaneous drop of the parenchymal perfusion of the left kidney compared to the right one. This is a sign of the exhaustion of the capacity of the epidural space and causes intracranial hypertension as shown by flow measurements of the medial cerebral artery (below). The details are shown in separate diagrams at the end of this report.
All the maneuvers to reduce the nausea do not influence the complete compression of the left renal vein between the aorta and the superior mesenteric artery.
The patient can repeatedly produce nausea and an impulse to vomit accompanied by headaches when she stretches her hips and drinks fluid. This substantially change is also the parenchyma perfusion of both kidneys as is outlined in the diagram at the end of this report.
After assuming an embryonic posture on her right side all the symptoms disappear within less than a minute and can be reinstituted by assuming a stretched body posture in a lying as well as in an upright position. The decisive condition to produce nausea is stretching of the hip joints, which by the way occurs also during the external rotation of the hip joints, and the subsequent pronounced lordosis of the lumbar spine.
Thus, the flexing of the hips with reduction of the lordosis provides prompt relieve from the symptoms of the left renal vein compression simultaneously with a decreased influx of left renal venous blood into the spinal canal. This is achieved by re-opening of the left common iliac vein. Thus, the pelvic collateral circulation of the still compressed left renal vein can now compensate the functional loss of the left renal vein and support the otherwise insufficient collateral pathway via the tronc reno-rachidièn.
The intracranial pressure increases when the patient feels nauseous. This can be demonstrated by an increasing resistance index of the right middle cerebral artery during development of nausea. In a position which prevents nausea (embryonic posture on her left side) the resistance index of the right middle cerebral artery is 0.47 and increases when she stretches her hips and feels nauseous and starts to vomit to 0.63.
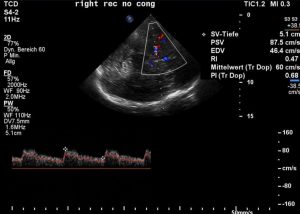
With flexed hips the diastolic flow velocity in the middle cerebral artery is 46,4 cm/s – the resistance index thus is 0,47 – the patient is free of symptoms
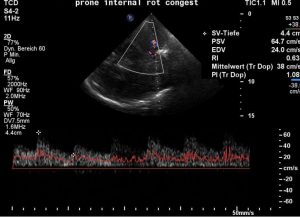
With stretched hips the diastolic flow velocity decreases to 24 cm/s, the RI rises to 0,63 – this is a sign of increasing intracranial pressure – causing headaches, nausea and vomiting. also the abdominal pain gets much worse
Thus, the influx of large amounts of left renal venous blood via the Tronc reno-rachidièn towards the epidural plexus is reflected by an increased intracranial pressure which simultaneously causes nausea.
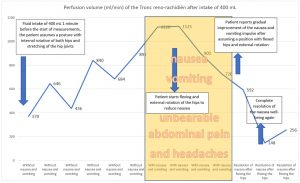
Timeline of the perfusion of the tronc réno-rachidièn: increasing volumes correlate to growing pressure inside the spinal canal and skull and are correlated to cerebral symptoms.
It is easily conceivable, that the increased pressure and volume of the epidural plexus is also responsible for the weakness of both legs. It is a common observation in well-developed collateral circulations via a Tronc reno-rachidièn, that neurological symptoms develop, starting in both legs.
The pathophysiological connection of left renal parenchymal perfusion and the collateral perfusion towards the epidural plexus and clinical symptoms of nausea and vomiting as well as the increased intracranial pressure is further reflected by the PixelFlux measurements of both kidneys under different conditions as outlined in the diagram below:
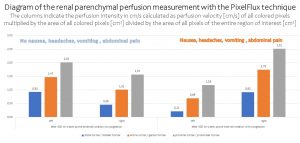
PixelFlux-measurements of both kidneys reveal a strict connection of reduced left renal perfusion as a sign of growing pressure inside the tronc réno-rachidièn and clinical symptoms. This underscores the eminent importance of functional blood flow measurements.
The coeliac trunk is found uncompressed (see table). Also, the superior mesenteric artery shows no sign of disturbed perfusion.
The splenic vein is compressed by the superior mesenteric artery which is pushed ventrally by the severe lumbar lordosis. A substantial flow acceleration result (see table).
Both femoral veins are significantly compressed at the crossing with the pubic bone. This compression is not substantially relieved by pure external rotation of the hips and may contribute to the congestion of both upper thighs.
Diagnoses
- Severe pelvic congestion
- May Thurner constellation which is resolved in an embryonic posture lying on the right or left side – Then all symptoms of nausea and increased intracranial pressure disappear
- Complete compression of the left renal vein. Massive lordogenetic compression with insufficient collateralization via a Tronc reno-rachidièn
- Splenic vein compression
- Severe lumbar lordosis
- Bilateral femoral vein compression at the crossing with the pubic bone
- No median arcuate ligament syndrome
- Clinical suspicion of a connective-tissue disorder which is synergistic with the lordogenetic venous compression syndromes
- Antiphospholipid syndrome
- Recurrent abortions
- Post-thrombotic state due to clotting disorder (see 8)
Recommendations
I recommended the surgical correction of the left renal vein compression but primarily of the compression of the left common iliac vein since it can be shown, that after assuming an embryonic posture, the left renal vein remains compressed with now flow while the left common iliac vein becomes decompressed and simultaneously all symptoms disappear.
Intraoperative Images

Exposed left renal vein, which is non-compressible. Yellow loops: suprarenal vein, patent branch of the left renal vein. Blue loop: tronc réno-rachidièn, which was the main collateral
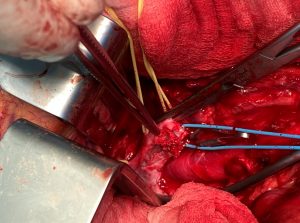
Left renal vein, dissected in longitudinal direction. The vein is filled with old and fresh thrombi due to glue inserted in the patient’s home country to obliterate the left ovarian vein.
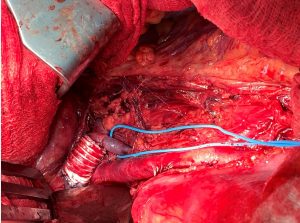
Operative result: replacement and prolongation of the left renal vein with a ring-enforced interposition graft. Preservation of the patency of the tronc-renorachidien.

External stent protecting the left common iliac vein against compression, because the patient also had a MAY-THURNER syndrome and suffered from chronic pelvic congestion syndrome. The ringenforced PTFE prosthesis is fixed by special techniques to the paravertebral fibrous tissue and the right iliac artery has to be kept in place too.
Result of the operation
The symptoms of the congestion of the brain (vomiting, headaches, and nausea) disappeared immediately.
Details and explanations
The possibility to measure the renal blood flow in different layers of the renal parenchyma with the PixelFlux technique offers unprecedented insights into the individual pathophysiology of the patients. Since the venous network of the retroperitoneum is individually very variable and may develop numerous collaterals the blood flow volume, its root and its effect are different from patient to patient despite similar compression syndromes.
One substantial advantage of this technique is that it can be applied in different body postures, during and after exercise and before and after the intake of food. Thus, the influence of changing body positions or the intake of food onto certain symptoms can be quantitatively related to the extent of the venous congestion. This cannot be achieved with any other existing technique today.
The capacity to develop collateral veins is substantially influenced by the age of the patient, the persistence of embryonic remnants of prenatal veins, the texture of the connective-tissue and the pressure within the different parts of the venous network.
The PixelFlux measurements of the renal parenchymal perfusion open a window to explain unexplained symptoms and combination of symptoms, even when they seem to be unrelated. The exact calculation of the blood flow within the kidneys is key to describe the hemodynamics of the collateral circulation in retroperitoneal and pelvic venous congestion syndromes. The reason is that the kidneys are extremely well-perfused. That is why already a slight compression of the left renal vein produces large volumes which need to be transported across collateral pathways. It depends on the capacity of the collateral pathways if the patient then remains healthy and without clinical symptoms. If the collateral pathways capacity is insufficient to transport all congested blood from the left kidney back to the heart, then the pressure inside the collateral network will increase. This is when symptoms start. The distension of the veins within the collateral circulation produces pain which images inside the distended wall of the veins. Here inflammatory reactions try to repair the micro structural damage which is produced by the severe distension of the previously small veins. These enlarging veins may also occupy more space. This may become symptomatic when these veins are in compartments where they cannot enlarge as required by the increasing collateral volume. Such compartments are the spinal canal, the perineural pouches of the spinal nerves, the Alcock canal of the pudendal nerve and the skull. In these compartments the pressure will increase due to the space-occupying and enlarging collateral veins. This pressurization will affect other organs and structures within these compartments.
So, a damage of spinal nerves or the spinal cord may develop, a pudendal neuralgia or an increased intracranial pressure.
The changing intracranial pressure can be checked by measuring the arterial perfusion of the median cerebral artery. The ratio of diastolic to systolic flow velocity within this vessel may increase when suddenly a volume shift from the left kidney towards the spinal canal is provoked by certain body postures.
In the patient presented here I could demonstrate a simultaneous increase of volume influx into the spinal canal via a tronc réno-rachidièn and the development of vomiting nausea and headaches as well as increasing abdominal pain. This was reflected by an increase of the resistance index (R I = (systolic flow velocity – diastolic flow velocity)/systolic flow velocity) of the median cerebral artery. Thus, a direct evidence was provided for the origin of vomiting and headaches generated by increasing intracranial pressure while a volume influx into the spinal canal could be quantified.
This volume influx became necessary since the tronc réno-rachidièn was the major collateral pathway of the compressed left renal vein and collateral veins along the embolized left ovarian vein heading towards the pelvis could not drain sufficient amounts of blood since the blood return towards the heart was obstructed due to a severe May-Thurner constellation.
When the patient then flexed her hips the changing position of the entire pelvis allowed a reopening of the left common iliac vein at the May Thurner point. The flexion of the hips reduces the anterior tilt of the entire pelvis, reduces the lumbar lordosis, and reduces the angle of the sacral bone with the longitudinal axis of the body. This is the reason why flexing the hips may reopen the compressed left common iliac vein. In the May Thurner syndrome, the left common iliac vein is uplifted by the erect position of the sacral bone. This is a consequence of the rotation of the entire pelvis around the transverse axis connecting both hip joints since the full stretching of the hip joints is already achieved at an angle of about 45° of the upper thigh with the longitudinal axis of the body. Such a position would not allow to lie supine with stretched hips or to stand upright. That is why further stretching of the hips is only possible by tilting the entire pelvis anteriorly and downward.
So the ultimate explanation for the enigmatic simultaneous occurrence of vomiting headaches, nausea, and abdominal pain which was only reduced by flexing the hips is the reduction of lordosis and anterior tilt of the pelvis which in turn eases the venous compressions in front of the spine and the sacral bone.
In this patient the left renal vein was completely obstructed in all body postures, but the left common iliac vein could be reopened by flexing the hips. This helped to reduce the influx of left renal venous blood into the spinal canal. Just this external volume entering the spinal canal was the reason for the increasing intracranial pressure whose well known clinical signs are nausea and vomiting as well as headaches.
Interestingly, the patient also reported increasing symptoms after the intake of fluids. This finds an explanation in the fact that fluid intake provokes a stronger renal perfusion which increases the collateral circulation towards the epidural plexus via the tronc réno-rachidièn.
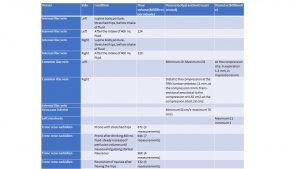
Table with perfusion details: