- संवहनी संपीड़न सिंड्रोम
- क्या आपका कोई सवाल है?
- चेकलिस्ट संवहनी संपीड़न सिंड्रोम
- महिला यौवन की मस्कुलोस्केलेटल विशेषताएं
- लॉर्डोसिस – कई उदर संपीड़न सिंड्रोम का कारण
- नटक्रैकर सिंड्रोम एक मिथ्या नाम है
- मे-थर्नर नक्षत्र / मे-थर्नर सिंड्रोम / कॉकटेल सिंड्रोम / वेना इलियाक संपीड़न सिंड्रोम
- पेल्विन्स कंजेशन सिंड्रोम (श्रोणि अंगों का जमाव)
- ट्रंकस कोएलियाकस संपीड़न / डनबर सिंड्रोम / MALS / लिगामेंट आर्किकेट सिंड्रोम
- विल्की सिंड्रोम / बेहतर मेसेन्टेरिक धमनी सिंड्रोम
- PixelFlux तकनीक का उपयोग करके संवहनी संपीड़न सिंड्रोम की मात्रा
- संवहनी संपीड़न सिंड्रोम में पुदाल तंत्रिकाशूल
- संवहनी संपीड़न सिंड्रोम का उपचार
- संवहनी संपीड़न सिंड्रोम जो मैंने हाल ही में खोजा है
- Kaleidoscope of instructive cases
- कार्यात्मक रंग डॉपलर अल्ट्रासाउंड – जैसा कि मैं इसे समझता हूं
- अनुसंधान
- विशेषज्ञता
- वैज्ञानिक सहयोग
- Cookie Policy
- Cookie Policy (EU)

Chronic regional pain syndrome with swelling of the right hand in a patient with a narrow subclavian vein valve at its junction with the pressurized internal jugular vein.
The 48-year-old female patient suffered a minor abrasion to the skin on the back of her right hand while gardening, immediately followed by painful swelling of the right hand, accompanied by restricted movement.
After an unremarkable X-ray examination of the hand, immobilisation and treatment with antibiotics and the painkiller ibuprofen were recommended. This had no effect. There is still pronounced swelling of the entire hand and almost complete restriction of movement in the wrist and all fingers. It is not possible to make a fist or extend the fingers. The hand is discoloured blue. The patient reports alternating sensations of cold and heat. The pain is very severe and has a neuropathic component in the form of hyperalgesia. In addition, there is a known, stable trigeminal neuralgia.
The patient’s medical history documents CRPS symptoms in the same arm many years ago, which were eliminated by resection of scar tissue on the subclavian vein. There were also pronounced CRPS symptoms in the left leg, which could be attributed to a May-Thurner syndrome. After decompression of the left pelvic vein and resection of the lumbar ganglion, the symptoms in the left leg also completely disappeared.
On the day of the examination, the patient’s right hand is trembling, swollen and very sensitive to pain.
The swelling extends to the distal third of the right forearm. The doughy, soft swelling shows no circumscribed hardening. There are no circumscribed skin changes externally.
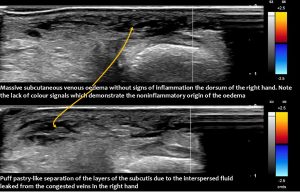
Quantitative colour Doppler sonography of both arms shows significant oedema in the area of the painful back of the right hand with puff pastry-like loosening of the subcutis due to deposited layers of fluid.
 The flow volume measurement in the brachial veins of both arms show no significant difference: 43 ml/min was measured on the right and 35 ml/min on the left. A particularly strong pulse is recorded in the right subclavian vein.
The flow volume measurement in the brachial veins of both arms show no significant difference: 43 ml/min was measured on the right and 35 ml/min on the left. A particularly strong pulse is recorded in the right subclavian vein.
This is caused by the intermittent closure of a valve at the junction of the subclavian vein and the internal jugular vein. This valve closes rhythmically, causing pulsatile modulation of blood flow.
In contrast, there is no such pronounced pulse in the left subclavian vein, nor is there a valve at the junction of the vein and the left internal jugular vein. Here, the blood flows into the jugular vein without any constriction.
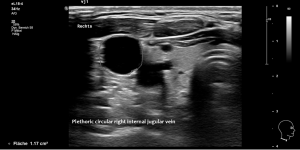
The right jugular vein is under significantly higher pressure, which can be seen from its round cross-sectional configuration.
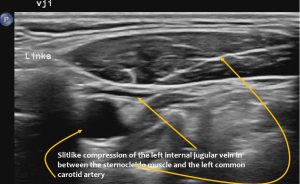
 On the left, however, the vein is narrow, oval in cross-section and obviously poorly filled due to its compression in between the common carotid artery and the sternocleidomastoid muscle.
On the left, however, the vein is narrow, oval in cross-section and obviously poorly filled due to its compression in between the common carotid artery and the sternocleidomastoid muscle.
The painful swelling of the right hand can therefore be associated with venous drainage obstruction from the right arm caused by the rhythmically closing valve. The valve closure is forced by increased pressure in the right jugular vein. There is apparently asymmetrical drainage of blood from the skull, with drainage via the right internal jugular vein being preferred.
Despite this obstruction of drainage, there is an undiminished volume flow from the arm into the central veins due to the venous back pressure in the right arm. This means that with a smaller cross-sectional diameter of the right subclavian vein compared to the left, the pressure in the right subclavian vein and thus in the upstream arm and hand veins must be significantly higher.
The sonographic findings thus allow the CRPS of the right hand to be interpreted as a consequence of asymmetrical drainage of the skull with compression of the opening of the right subclavian vein into the right internal jugular vein. The valve of the subclavian vein protrudes into the jugular vein and is clamped there.
The rhythmic pressure fluctuations in the right jugular vein are caused by the pulse of the right atrium, which propagates into the distended jugular vein and thus rhythmically compresses the valve of the subclavian vein.
Similar case reports were found in the medical literature:
CUCCI CE, BOTTINO CG, CIAMPA V. VENOUS OBSTRUCTION OF THE UPPER EXTREMITY CAUSED BY A MALFORMED VALVE OF THE SUBCLAVIAN VEIN. Circulation. 1963 Feb;27:275-8. doi: 10.1161/01.cir.27.2.275. PMID: 14173496.
https://pubmed.ncbi.nlm.nih.gov/14173496/
This article describes a 39-year-old man who, as a warehouse worker, developed swelling of the left arm with bluish discolouration and pain, as well as functional impairment. The venous pressure in the left basilar vein (elbow vein) was twice as high as in the right, namely 7.8 mmHg.
Phlebography showed an abrupt interruption of the subclavian vein:
Liao J, Wu Z. Venous obstruction of the upper extremity caused by subclavian vein valve hypertrophy. Interdiscip Cardiovasc Thorac Surg. 2024 Oct 8;39(4):ivae165. doi: 10.1093/icvts/ivae165. PMID: 39348191; PMCID: PMC11648952.
https://pubmed.ncbi.nlm.nih.gov/39348191/
This article describes a 26-year-old man who had developed swelling of the right arm over a period of years, accompanied by bluish discolouration and pain, which increased significantly when washing his hands. He also described a feeling of heaviness in his arm. The cause of the venous outflow obstruction was a thickened valve in the subclavian vein at its junction with the jugular vein/brachiocephalic vein. The patient was successfully treated with stent implantation.