- Nouveaux articles
- Cabinet médical / Prise de rendez-vous en ligne
- Syndrome de compression vasculaire
- Avez-vous des questions ?
- Liste de contrôle des syndromes de compression vasculaire
- Constellation de May-Thurner / Cockett’s syndrome
- Syndrome de la ligne médiane
- Syndrome de congestion pelvienne
- Syndrome de compression du tronc coeliaque – Syndrome de Dunbar – Syndrome du ligament arqué médian – MALS
- Syndrome de Wilkie / syndrome de l’artère mésentérique supérieure
- Compression de la veine cave inférieure
- Névralgie pudendale dans les syndromes de compression vasculaire
- Traitement des syndromes de compression vasculaire
- Syndromes de compression vasculaire I récemment détectés
- Un kaléidoscope de cas instructifs
- Diagnostic ultrasons
- L’échographie Doppler couleur fonctionnelle – comment je m’y prends
- Qualifications, expériences et compétences
- Collaboration scientifique
- Cookie Policy
- Cookie Policy (EU)
- Impressum

Essoufflement insupportable dépendant de la posture et plénitude dans la partie supérieure droite de l’abdomen dus à une compression diaphragmatique variable des veines hépatiques et de la veine cave inférieure.
The patient, a slender woman of 65 years, suffers from breathlessness and massive tension and fullness in the right upper abdomen as soon as she needs to bend forward or lies on her left side. This developed after a bicycle accident 3 years ago when she fell on her right sided thorax. 7 years ago she was operated on recurrent pneumothoraces on the right side for which a pleural endometriosis was found being responsible.
After this operation no problems with breathing occurred until the accident 3 years ago.
A repeated CT of the thorax, an MRI of the trunk and abdomen as well as ultrasound of the abdomen did not reveal any cause of her complaints. Since she also wakes up at night sweating breathless and with tachycardia and arrhythmia her symptoms finally have been classified as psychosomatic. She is desparate since she cannot work in a hotel anymore where she needs to cover beds requiring a bending forward.
The ultrasound examination of the liver and its vessels but demonstrated a reason for her complaints. The diaphragm was compressing the mouth of the hepatic veins as well as the vena cava inferior as soon as the patient assumed those positions which were very unpleasant and caused her breathlessness.
This was bending forward while being upright (sitting or standing) and lying horizontally on her left side. Then a massive flow acceleration within the confluence of the hepatic veins could be demonstrated up to more than 310 cm/s whereas in the central portions of the liver veins the flow velocity was as low as 13 cm/s.
 A similar flow acceleration was found in the vena cava inferior due to its compression by the diaphragm.
A similar flow acceleration was found in the vena cava inferior due to its compression by the diaphragm.
Moreover, the liver was found compressed by 2 ribs which squeezed the right liver lobe when the patient was bending forward impressing its surface by 14 mm. This liver compression was also affecting the compression of the vena cava inferior.
The liver was also slightly swollen with a height of 16.6 cm (normal less than 13 cm).
Since the patient also had slightly elevated liver enzymes (ALAT) a low-grade liver damage by the above-mentioned mechanisms can be assumed since conventional reasons for elevated liver enzymes as infections or toxic damages had been ruled out.
The pleura of the right lung was unremarkable during the sonographic examination.
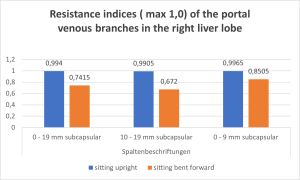
The tenderness and fullness in the right hypochondrium is explained by the suddenly increasing tension of the liver due to the posture-dependent venous congestion of this organ. This could be demonstrated by liver parenchyma perfusion measurement with the PixelFlux technique. The small subcapsular branches of the portal vein showed a high pulsatility and reduced venous volume as long as the patient was comfortable while being upright or lying horizontally on her back. This points to an easy passage of portal blood via the liver parenchyma to the hepatic veins since their outflow was only little constricted by the diaphragm.
When she provoked her symptoms by turning to her left side while lying horizontally or bending over while sitting her symptoms with breathlessness and fullness in the right hypochondrium developed within seconds while the parenchymal liver veins dilated and became congested.
Their pulsatility was suddenly reduced since the sudden massive congestion did not allow a rhythmic outflow via the liver veins anymore.
This sudden blockage of flow from the lower hemisphere to the heart explains the posture-dependent tachycardia and arrhythmias and may contribute to breathlessness due to a suddenly reduced lung perfusion.