- El consultorio / Programación de citas en línea
- Compresiones vasculares
- ¿Tiene alguna pregunta?
- Lista de control Síndromes de compresión vascular
- Lordosis – Causa de numerosos síndromes de compresión abdominal
- Síndrome de May-Thurner/ síndrome de Cockett/ síndrome de compresión de la vena ilíaca
- Síndrome de la línea media (síndrome de congestión de la línea media)
- Síndrome de congestión pélvica (congestión de los órganos pélvicos)
- Compresión del tronco celíaco /síndrome de Dunbar/ síndrome de AMS/ síndrome del ligamento arcuato
- Síndrome de Wilkie/ síndrome de la arteria mesentérica superior
- Compresión de la vena cava inferior
- Neuralgia púdica en los síndromes de compresión vascular
- Tratamiento de los síndromes de compresión vascular
- Síndromes de compresión vascular que he detectado recientemente
- Kaleidoscope of instructive cases
- Servicios
- Ultrasonido Doppler color funcional – lo que entiendo por esto
- Medición de la circulación sanguínea – Método PixelFlux
- Investigación
- Perfil
- Infección por virus Borna
- Colaboración científica
- Cookie Policy
- Cookie Policy (EU)

Successful treatment of a teenage girl who was unable to eat due to extreme postprandial pain and unable to walk due to spasticity in her left leg
The 14-year-old girl had been healthy until the age of 11, when she was diagnosed with dysautonomia and POTS.
At 13, she contracted the Corona virus for the second time and soon developed severe chest pain, requiring hospitalisation. This pain was interpreted as costochondritis. In the first few days after admission, she lost the ability to swallow. She was unable to swallow food, medication or even water and was diagnosed with ‘functional dysphagia’. Initially, it was assumed that she was suffering from an eating disorder involving food avoidance, so she was fitted with a nasal feeding tube. Within a few weeks of losing her ability to swallow, she began to experience stomach pain during enteral feeding. She experienced severe, excruciating pain when the tube was flushed, as well as pain radiating to both flanks. This pain was so severe that she could only be fed at night while she was asleep, and only a small amount of food could be given at a time. Eventually, she started vomiting continuously and had to switch from tube feeding to total parenteral nutrition during her six-month hospital stay. A few weeks after admission, she developed severe pain in her upper left abdomen and left flank, and her left leg became numb. Spastic internal rotation of the leg in the hip joint developed — the patient was now unable to walk and was confined to a wheelchair. Over the following eight months, the painful spasticity in her leg worsened to such an extent that she was unable to sit, stand or walk. She became completely bedridden. At this point, the attending physicians interpreted the pain as ‘pain hypersensitivity’ and the inability to eat due to pain as ‘functional dysphagia’. They initiated symptomatic therapy with opioids, analgesics and antidepressants, and used an antipsychotic for extreme pain crises as they believed this to be a psychiatric disorder. During her further hospitalisation, she developed numerous complications, including sepsis originating from the central venous catheter for parenteral nutrition, an abdominal wall infection at the site of the transcutaneous feeding tube insertion, non-specific colitis lasting one month, urinary problems and an oculogyric crisis. She was unable to eat orally for over six months and did not gain any weight for over 18 months.
Upon presentation here, numerous vascular compression syndromes were diagnosed.
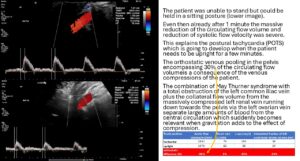
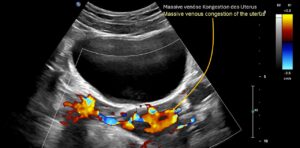
- There was complete compression of the left common iliac vein, leading to massive congestion of the pelvic organs

- 50% of the congested blood volume was collateralised to the spinal canal via the left ascending lumbar vein.
- Severe compression of the left renal vein.

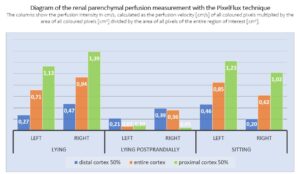
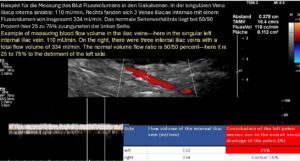
The PixelFlux measurement clearly demonstrates the insufficiency of the collateral pathways of the left renal vein while the patient is lying fasting. The perfusion of the left kidney is then only 76% of that of the right kidney.
While lying postprandially, severe suppression of perfusion in both kidneys is evident, with the left kidney receiving only 20% of the severely reduced blood flow of the right kidney. Sitting while fasting impedes blood flow to the right kidney. Such precise statements about haemodynamic effects and blood flow distribution volumes can only be made using the PixelFlux technique. - the clinically suspected compression of the duodenum between the aorta and the superior mesenteric artery could not be investigated due to the patient’s complete inability to take anything orally – a Wilkie syndrome was therefore clinically assumed.
The clinically suspected and intraoperatively confirmed tronc réno-rachidièn could not initially be visualised sonographically, as the high congestive pressure of the spinal canal meant that there was no effective blood flow that would have produced a Doppler signal. This was an expression of the enormous intraspinal pressure, which corresponded to the pressure in the compressed left renal vein.
Furthermore, the congestion pressure in the spinal canal was increased by large amounts of blood via the ascending lumbar vein on the left, resulting in neurological deficits in the form of extremely painful spasticity in the left leg.
The spastic internal rotation of the left leg is caused by venous congestion of the spinal cord in the spinal canal, while pain radiating along the sciatic nerve is caused by severe obstruction of drainage in the left internal iliac vein, which almost completely stops venous return from the sciatic nerve via the left inferior gluteal vein.
The pain on ingestion was easily explained by the increase in pressure exerted by the filling, enlarging stomach on the massively congested left renal vein behind the stomach during oral ingestion. From a clinical point of view, there was also compression of the duodenum (Wilkie syndrome), which caused prompt vomiting after food intake in combination with severe pain in the upper abdomen.
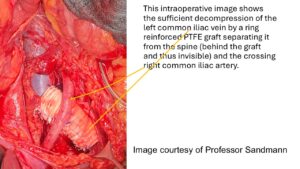
The patient’s vascular compression was eliminated by relieving pressure from the spine and surrounding intestines on both the left renal vein and the left common iliac vein using a ring-reinforced PTFE sleeve (Professor Sandmann, Klinik Beletage Düsseldorf).
Covering the left renal vein also protects the duodenum, which, in cases of severe lumbar lordosis, is compressed between the aorta and superior mesenteric artery when crossing the aorta, in the same way as the left renal vein.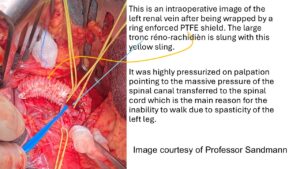
The decompression had an immediate positive effect on the patient’s symptoms. Just a few days after the operation, the patient was able to extend her left leg from spastic internal rotation.
On the seventh postoperative day, she stood up, and within ten days she began to walk again.
Within two weeks, she was eating and drinking, and was able to feed herself completely orally. The patient became completely pain-free, so all medication could be stopped!
Seven weeks after the operation, she was able to fly home overseas.